Managing and Treating Cirrhosis
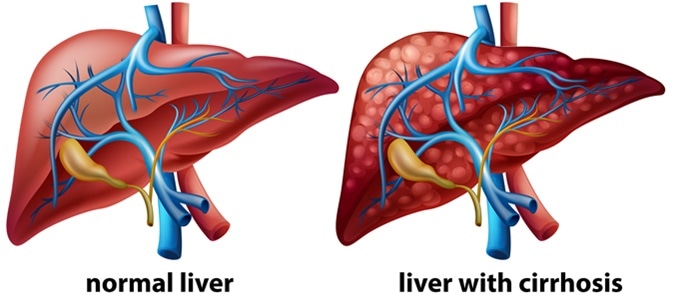
Liver cirrhosis is defined as the last stage of long-term liver disease, and is a leading cause of morbidity worldwide. The condition is characterized by liver scarring, which is the replacement of healthy liver tissue by scar tissue. Fibrosis is the specific term used to represent this process. Scarred tissues cause permanent damage to the liver and prevent it from working normally. The distorted tissue also blocks the hepatic and portal blood flow. Disruption of blood flow through the liver ultimately leads to liver failure.
What are the main causes of cirrhosis?
The main causes of cirrhosis in developed countries like the USA include hepatitis C virus infection, excessive alcohol consumption and non-alcoholic liver disease. On the other hand, the hepatitis B virus is the most common causative agent in African and Asian countries.
What are the signs and symptoms of cirrhosis?
Cirrhosis is initially asymptomatic and the condition may present at a stage when the liver is severely damaged. In some cases, abnormal liver function tests or radiological findings may suggest further evaluations such as a biopsy, which leads to the diagnosis being made at an earlier stage when intervention may be successful. Screening for liver abnormalities at regular intervals is highly recommended.
What are the complications associated with cirrhosis?
Some of the critical consequences of cirrhosis include the following:
- Variceal bleeding – Abnormal bleeding from dilated tortuous veins in the portal system draining the liver, due to portal hypertension
- Ascites – Accumulation of fluid in the abdomen
- Bacterial peritonitis – Infection of ascitic fluid
- Encephalopathy – Brain damage due to the build-up of toxins as a result of liver dysfunction.
Management and treatment of cirrhosis
The management of cirrhosis depends on the state of the liver, i.e. whether it is compensated or decompensated.
- When it is compensated, the main focus is on the prevention of variceal hemorrhage which could result in the progression to decompensation.
- The decompensated state is represented by the presence of acute variceal haemorrhage, ascites, encephalopathy and jaundice in various combinations. These situations generally require prompt hospitalization as they may be rapidly fatal.
Hepatorenal syndrome is a frequent complication often found in hospitalized patients. It is the end-result of the alterations in the blood flow involving various organs of the body that are caused by cirrhosis. The final outcome of these abnormal hemodynamics is fluid build-up in the abdomen, a condition termed ascites, upon which hepatorenal syndrome may supervene. The management at this stage therefore follows the treatment algorithm prescribed for ascites.
Excessive alcohol consumption paves the way for fibrosis and finally decompensation of the liver. Patients who suffer from alcoholic cirrhosis should abstain from alcohol. The initial period of alcohol abstinence is hard on the liver because of the known immunosuppressive effect of alcohol.
Pharmacological treatment
Interferon-based therapies are the treatment of choice for patients suffering from HCV-cirrhosis. Oral nucleoside and nucleotide inhibitors of hepatitis B virus polymerase are the drugs of choice for cirrhosis due to hepatitis B virus.
Hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is the number one cause of death due to liver cirrhosis. Hence patients with cirrhosis should undergo timely screening for HCC. Global clinical guidelines such as those issued by the American Association for the Study of Liver Disease (AASLD) and the European Association for the Study of the Liver (EASL) recommend at least yearly HCC screening in such patients. Ultrasound imaging, computed tomography (CT) scans and magnetic resonance imaging (MRI) are commonly used for screening HCC.
In case HCC is detected, the treatment algorithm usually depends on the size and number of the tumors. Surgery is the best option for HCC; however, it is not tolerated by patients with cirrhosis. For people with HCC due to cirrhosis, liver transplantation is generally recommended.
Some other treatments options for HCC due to cirrhosis, which are not suitable for liver transplantation or resection, include:
- Radiofrequency ablation
- Chemoembolization
- Alcohol ablation
- Cyberknife radiotherapy
Liver transplantation
Liver transplantation is the last resort for end-stage cirrhosis. Recent years have witnessed enormous progress in liver transplantation. Improved immunosuppressive agents have led to a decreased number of organ rejections. However, recurrent HCV infection and adverse effects associated with the long-term use of immunosuppressive agents are major issues.
Future directions
Emerging research in the field of cirrhosis and end-stage liver disease has resulted in a paradigm shift in the management of this condition. The main focus of today’s research is to treat the root cause of cirrhosis and manage portal hypertension effectively. Improved screening tests for early detection of fibrosis, and the use of stem-cell therapy or hepatocyte transplantation to promote liver regeneration, are some other promising fields of research.
Sources
- https://www.ncbi.nlm.nih.gov/pubmed/19455106
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2271178/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5339475/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5680752/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3098395/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017060/
Further Reading
- All Cirrhosis Content
- What is Cirrhosis?
- What Causes Cirrhosis?
- Liver Disease Symptoms
Last Updated: Mar 20, 2019
Source: Read Full Article



