Inflammatory Bowel Disease Is on the Rise in Canada
The prevalence and incidence of inflammatory bowel disease (IBD), which consists of Crohn’s disease and ulcerative colitis, is increasing in Canada, according to a new report. IBD is likely to become a significant burden to the healthcare system unless measures are enacted to ensure that the growing number of patients get the care they need, the authors wrote.
A six-province study led by the Canadian Gastro-Intestinal Epidemiology Consortium found that the prevalence of IBD has climbed precipitously since 2002. In that year, the prevalence was 400 per 100,000 individuals. By 2014, it had risen to 636 per 100,000.
“Crohn’s disease and ulcerative colitis are global diseases, with Canada reporting among the highest prevalence and incidence of IBD in the world,” lead author Stephanie Coward, PhD, an IBD epidemiology researcher at the University of Calgary’s Cumming School of Medicine in Alberta, told Medscape Medical News.
The report was published online September 5 in the Journal of the Canadian Association of Gastroenterology.
Healthcare Costs Rising
About 322,600 people in Canada are estimated to have IBD, and this number is expected to rise by 2.4% per year. By 2035, 470,000 Canadians are predicted to have IBD, according to the researchers.

Dr Stephanie Coward
The overall incidence of IBD is also climbing. The current incidence is 30 per 100,000 person-years, indicating that more than 11,000 Canadians will be newly diagnosed with IBD in 2023. The incidence is projected to rise by 0.58% per year, reaching 32.1 per 100,000 person-years by 2035. “Decades of rising incidence, in conjunction with low mortality, means that individuals with IBD are continually added to gastroenterology clinics, whereas few leave. The Canadian healthcare system needs to contend with that ongoing rise to ensure that these patients receive the care they need,” said Coward.
IBD is diagnosed predominantly in children, although it can be diagnosed at any age, senior author Gilaad G. Kaplan, MD, MPH, professor of medicine at the Cumming School of Medicine, told Medscape.
“Because it’s a chronic disease, you can’t be cured of it,” he added. “Our forecasting models predict that roughly 1% of the Canadian population will be living with IBD in the next 10 years.”

Dr Gilaad Kaplan
It is not just the volume of people with IBD, but also the aging population that is creating a challenge to gastroenterology clinics, said Kaplan. “Seniors represent the fastest-growing demographic of people living with IBD. Say you were diagnosed with Crohn’s disease in the 1990s when you were in your 30s. You are now in your 60s and may have some age-related comorbidities. So now, we’re not just caring for the IBD and its complications, but also having to do it in the context of age-related comorbidities such as diabetes, cancer, and cardiovascular disease, which adds a whole other layer of complexity.”
Scientific understanding of the pathogenesis of IBD has greatly improved, allowing researchers to develop new treatments and therapies. “But they are complex, they require a certain level of expertise on the part of the physician, and they’re quite costly,” said Kaplan. “The use of these drugs is increasing year after year, which is fantastic, but it ends up causing a strain from a healthcare perspective, because the cost of delivering care is rising.”
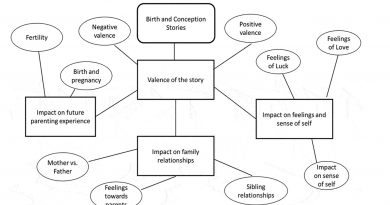
One solution is to redesign how healthcare is delivered, especially with regard to the special needs of patients with IBD, Kaplan added. “One of the things we discovered in the report was that there is a tremendous mental health burden associated with IBD, which tells us that a multidisciplinary approach is essential. In our clinic, we have social workers, counselors, nurse practitioners, gastroenterologists, and dietitians to address all the different facets of the disease.”
Access to care can be difficult for some patients. To address this problem, Kaplan suggests the adoption of virtual hybrid clinics when appropriate. “People of lower socioeconomic status may not be able to take time away from work. People who live in rural areas may find it difficult to make it to the clinic in person. And seniors may have age-related difficulties getting to us. We learned from the pandemic that we could integrate virtual care and remote monitoring of patients, so a hybrid virtual clinic might help improve access to care. A lot of times, all we need to do is have a conversation. Other times, we need to do tests that require patients to come into the healthcare system.”
“A Tremendous Burden”
Commenting on the study for Medscape, Brian Bressler, MD, founder of the IBD Centre of British Columbia and clinical associate professor of medicine at the University of British Columbia in Vancouver, said that the increase in IBD and its growing burden on Canada’s healthcare system come as no surprise.
“We see a tremendous burden in our province,” said Bressler. “We have a tremendous amount of requests for gastroenterologists to be involved with patient care, so we are seeing a lot of IBD, and it seems that there is more of it now than years ago. What the report says really rings true.”

Dr Brian Bressler
Bressler endorses the use of multidisciplinary clinics. “At our center, we focus on managing these challenging patients with a team approach. We work very carefully and closely with IBD-focused nurses: nurse practitioners who are involved in the care in some instances. We have a pharmacist, a dietitian, clinical counselors, a psychiatrist, and multiple people involved. Our patients require attention to their entire well-being, not just the inflammation in their bowel.”
The report was funded by AbbVie Corporation, Janssen Canada, Pfizer Canada, Bristol Myers Squibb Canada, Amgen Canada, and Takeda. Coward and Bressler reported no relevant financial relationships. Kaplan has received honoraria for speaking or consultancy from AbbVie, Janssen, Pfizer, and Takeda. He has received research support from Ferring, Janssen, AbbVie, GlaxoSmithKline, Merck, and Shire. He also has been a consultant for Gilead.
J Can Assoc Gastroenterol. Published September 5, 2023. Full text
For more news, follow Medscape on Facebook, X (formerly Twitter), Instagram, YouTube, and LinkedIn
Source: Read Full Article