Study supports evidence that ivermectin is ineffective at treating COVID-19
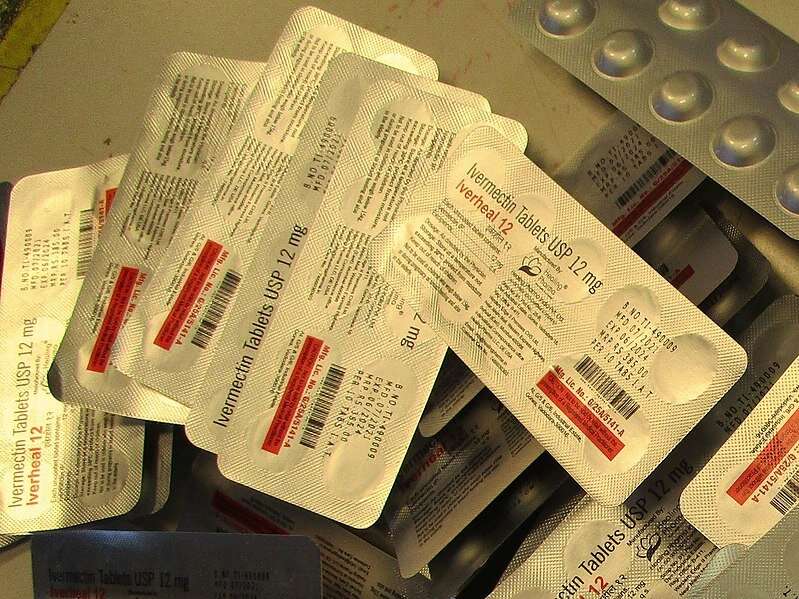
High doses of the drug ivermectin, controversially recommended by some high-profile political and media figures during the COVID-19 pandemic, is ineffective at treating the COVID-19 virus, say University of Oxford- affiliated researchers in a study published today in eLife.
The study was conducted mainly in the Hospital for Tropical Diseases in Bangkok. It is part of the ongoing PLATCOV trial—a phase 2 multi-center platform that requires a comparatively small sample size to assess the antiviral pharmacodynamics and effectiveness of medicines in treating early symptomatic COVID-19 infections.
The findings support claims that the drug has little antiviral activity against SARS-CoV-2—and help resolve the controversy about the effectiveness of ivermectin in treating COVID-19.
“Our study shows there is no support for the continued use of ivermectin in treating COVID-19,” says senior author and PLATCOV co-PI Prof Sir Nicholas White, Professor of Tropical Medicine at the Mahidol Oxford Tropical Medicine Research Unit (MORU), Mahidol University, Bangkok, Thailand, and the Center for Tropical Medicine and Global Health (CTMGH), Nuffield Department of Medicine, University of Oxford, U.K.
Several different drugs have been suggested for the early treatment of COVID-19. Monoclonal antibodies, a type of targeted drug therapy, have been shown to be effective in preventing and treating COVID-19. However, they are expensive and they require an intravenous injection to be administered. Similarly, the new drugs molnupiravir and nirmatrelvir have shown promise in clinical settings, but they are largely unavailable outside of high-income settings.
Repurposed drugs, such as ivermectin, have therefore been explored in treating COVID-19, as they are more affordable and generally available. However, trials of these drugs have often been flawed and/or underpowered. This has led to uncertainty and confusion over the effectiveness of these drugs, especially in the case of ivermectin.
“Even now, three years after the start of the pandemic, it remains uncertain whether any of the proposed repurposed antiviral treatments are effective at fighting COVID-19, highlighting the limitations of the tools currently used to assess these drugs,” explains co-lead author Dr. William Schilling, Research Physician at MORU and CTMGH. Schilling contributed equally alongside fellow co-lead author Podjanee Jittamala, a lecturer in the Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University.
To quantify the effectiveness of ivermectin against COVID-19, the team used the PLATCOV trial to compare the rates at which different drugs reduced the viral load of SARS-CoV-2 from patients. The study participants were previously healthy adults between the ages of 18–50 with early, symptomatic COVID-19.
Participants were randomized to one of six treatment schedules. There were 205 patients in total; 46 were given a high dose of oral ivermectin daily for a week; 40 were administered the monoclonal antibodies casirivimab and imdevimab (10 prespecified as unblinded for the analysis); 45 received no drugs and the remainder were randomized to other drugs. Swabs were taken serially from the participants’ tonsils throughout the course of the study (20 in total per person), allowing the researchers to characterize the decline in the viral load of SARS-CoV-2.
In patients treated with ivermectin, the average estimated rate of SARS-CoV-2 viral clearance was 9.1% slower than in those treated with the non-study drugs. Those treated with casirivimab/imdevimab had a viral clearance rate that was 52.3% faster than in those treated with the non-study drugs, consistent with the proven clinical benefit of this medicine against susceptible viruses.
These results suggest that ivermectin does not have measurable antiviral activity in early symptomatic COVID-19. The positive preliminary results from casirivimab/imdevimab confirmed that PLATCOV is able to identify treatments with clinically relevant antiviral effects against COVID-19.
“PLATCOV is a relatively simple method of assessment, requiring only a small number of volunteer patients to quantify the effectiveness of a drug,” explains Dr. Podjanee Jittamala. “The procedures are well tolerated—they have few adverse effects—and tonsil swabs are much better tolerated than swabs taken from deep inside the nose.”
Further studies are warranted to confirm whether the daily sampling schedule used in the current work strikes the optimal balance between collecting as much information as possible while maintaining the tolerability of the trial for patients. There was substantial variability in the estimated viral loads, which may be reduced in further studies by accounting for the variable volumes absorbed by the swabs or by using a different sampling technique.
The PLATCOV methodology used in the study could become a standardized method of determining the effectiveness of drugs against COVID-19, and potentially other respiratory tract infections—and so could become an important public health tool for policymakers and political leaders.
“The rapid and efficient characterization and comparison of potential antiviral therapeutics in COVID-19 is important for policy recommendations, particularly while cost and availability limit access. The method described in our study shows great promise for assessing antiviral effectiveness, not just in COVID-19, but potentially in other common or epidemic respiratory illnesses such as influenza,” says Prof White.
More information:
William HK Schilling et al, Pharmacometrics of high dose ivermectin in early COVID-19: an open label, randomized, controlled adaptive platform trial (PLATCOV), eLife (2023). DOI: 10.7554/eLife.83201
Journal information:
eLife
Source: Read Full Article



