Study finds ‘shared care’ is preferred by patients, is cheaper and just as effective
A new study led by researchers at Peter Mac has found sharing follow-up care between a GP and hospital-based specialists was preferred by bowel cancer patients, was cheaper for the health care system and was just as effective as standard hospital-based care.
The SCORE (Shared Care follow-up for colOREctal cancer survivors) trial was the largest study of shared care follow-up for cancer survivors, and the only study of shared care for people who have been treated for bowel cancer.
The study has just published online in eClinicalMedicine and was previously presented at the annual meeting of the American Society of Clinical Oncology, the world’s largest clinical cancer conference, held in Chicago in June.
The trial enrolled 150 patients who had just completed their bowel cancer treatment—involving surgery and, for most, also chemotherapy and radiotherapy—at Peter Mac or four other hospitals across Melbourne.
For their follow-up appointments every three months, patients were randomized to have these either with hospital-based specialists (the current standard of care) or to a model where alternate visits were with the patient’s usual GP.
Professor Michael Jefford said the results supported a wider roll-out shared care—a model used for managing pregnant women and people with asthma, diabetes and heart disease in the community, but not for recovery from cancer.
“Shared care is a model where roles and responsibilities are shared between hospital specialists and GPs,” says Prof Jefford, who led the study and is an oncologist and Director of the Australian Cancer Survivorship Center at Peter Mac.
“Our study shows that shared care is acceptable, safe, preferred by bowel cancer patients, and is cheaper for the health care system. We now need to focus on widespread implementation of this effective model.”
Patients and GPs in the shared care arm received information about the post-treatment phase, and GPs received brief management guidelines.
Patient “quality of life” was the same regardless of shared or hospital-based care, meeting the aim to the trial. Patient satisfaction and unmet needs were similar, and there was also no difference in cancer recurrence.
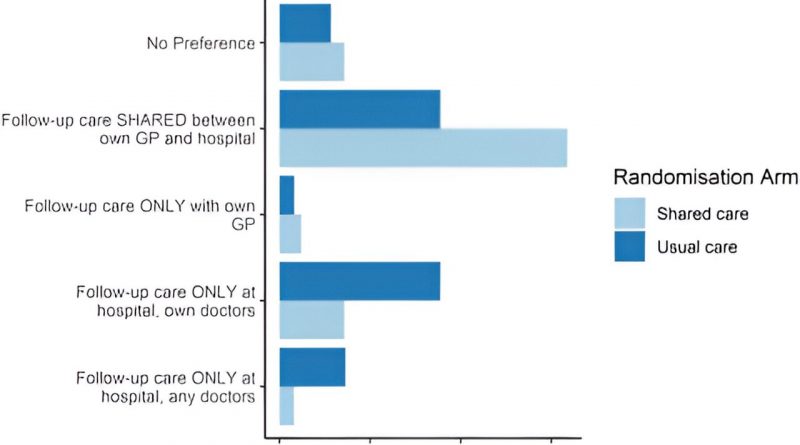
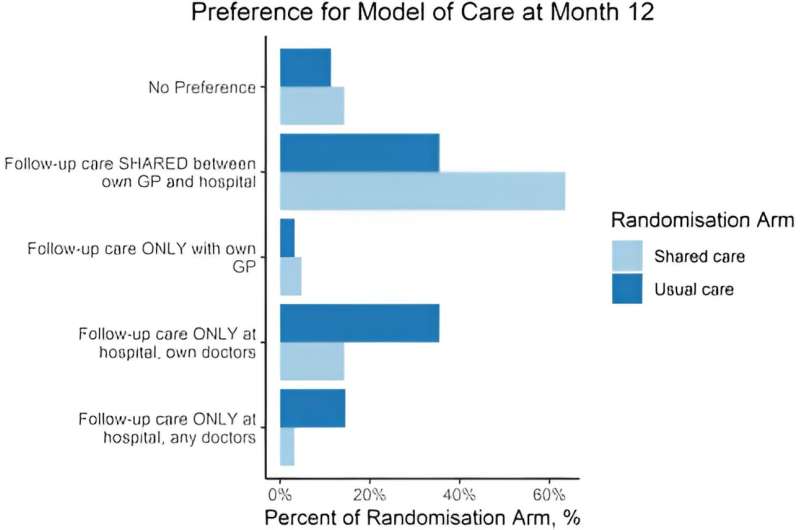
GPs were more likely to do recommended tests, while Medicare data showed that shared care was cheaper. Patients who received shared care had a strong preference for this model, while those who received hospital-based care had an equal preference for either.
Prof Jefford says the trial “responds to recommendations to investigate shared care models for cancer survivors,” noting the recent Australian Cancer Plan highlighted this as a potential response to cost and capacity constraints.
More information:
Michael Jefford et al, SCORE: a randomised controlled trial evaluating shared care (general practitioner and oncologist) follow-up compared to usual oncologist follow-up for survivors of colorectal cancer, eClinicalMedicine (2023). DOI: 10.1016/j.eclinm.2023.102346
Journal information:
EClinicalMedicine
Source: Read Full Article