Simulation-Based Training Effective for Transesophageal Echo
Simulation-based teaching of transesophageal echocardiography (TEE) improved cardiology fellows’ knowledge, skills, and comfort with the procedure compared with traditional training, a new study shows.
“TEE learning may be hampered by the lack of availability of teachers and equipment and by the need for esophageal intubation, which is semi-invasive,” Augustin Coisne, MD, PhD, of the Cardiovascular Research Foundation in New York City, told theheart.org | Medscape Cardiology. “In this setting, simulation emerges as a key educational tool, but we were lacking evidence supporting simulation-based educational programs.”

Fellows in the simulation group achieved higher theoretical test scores and practical test scores after the training than did those in the traditional group.
Furthermore, Coisne said, “The results of the subgroup analyses were surprising and unexpected. The effect of the simulation-based training was greater among fellows at the beginning of fellowship ― ie, 2 years or less of training ― in both theorical and practical tests and in women [vs men] for the theoretical test.”
Their results, from the randomized SIMULATOR study, were published online January 11 in JAMA Cardiology.
More Ready, More Confident
The researchers randomly assigned 324 cardiology fellows (mean age, 26.4 years; about 30% women) inexperienced in TEE from 42 French university centers to TEE training with or without simulation support. Both groups participated in traditional didactic training using e-learning with an online course that is compulsory for all cardiology fellows in France.

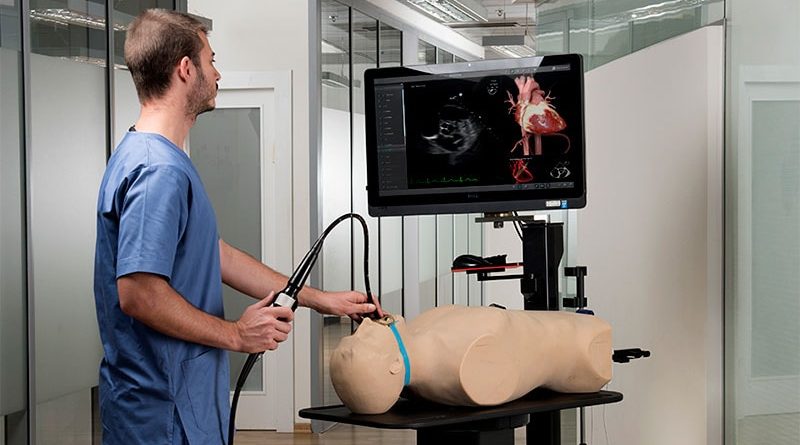
The simulation group also participated in two 2-hour teaching sessions using a TEE simulator.
Each fellow completed a theoretical and a practical test prior to training to assess their baseline TEE level and again 3 months after the end of the training program. A TEE simulator (U/S Mentor Simulator; 3D Systems Simbionix) was used for all tests, and 24 certified echocardiography teachers served as both trainers and raters.
The theoretical tests included 20 online video-based questions to evaluate recognition of standard TEE views, normal anatomy, and some pathologic cases. Fellows had 90 seconds to choose the best answer for each question from five multiple-choice options.
For the practical tests, fellows had 3 minutes to familiarize themselves with the handling of the simulator, without specific training and before the probe introduction.
They were asked to show 10 basic views on the simulator and had a maximum of 1 minute for each view.
The co-primary outcomes were the scores in the final theoretical and practical tests. TEE duration and the fellows’ self-assessment of their proficiency were also evaluated.
At baseline, the theoretical and practical test scores were similar between the groups (33.0 for the simulator group vs 32.5 for the traditional group, and 44.2 vs 46.1, respectively).
After training, the fellows in the simulation group had higher theoretical and practical test scores than those in the traditional group (47.2% vs 38.3% and 74.5% vs
59.0%, respectively).
Score changes were consistently higher when the pretraining scores were lower, an association that was stronger in the simulation group.
Coisne noted that subgroup analyses showed that the effectiveness of the simulation training was greater when performed at the beginning of the fellowship. On the theoretical test, the point increase was 11.9 for the simulation group vs 4.25 points for the traditional training group; for the practical test, the increases were 24.0 points vs 10.1 points.
After training, it took significantly less time for the simulation group to complete a TEE than it did the traditional group (8.3 vs 9.4 minutes).
Furthermore, simulation group fellows reported that they felt more ready (mean score, 3.0 vs 1.7) and more confident (mean score, 3.3 vs 2.4) about performing a TEE alone after training.
“The simulation approach is definitively scalable to every institution,” Coisne said. “However, a medico-economic analysis should be interesting because the cost of the simulator and its maintenance might be a limitation to spread simulation-based teaching. The possibility for smaller hospitals to pool their financial input to share a TEE simulator could be considered to increase its cost-effectiveness.”
Real-World Outcomes Required
Commenting on the study for theheart.org | Medscape Cardiology, S. Justin Szawlewicz, MD, chair of cardiovascular medicine at Deborah Heart and Lung Center in Brown Mills, New Jersey, pointed out that the authors indicated that the number of TEEs performed by the trainees was not collected.
“This would be useful information to determine if those who received simulator training sought out and performed more TEEs, and also to determine if cardiology trainees in France perform a similar number of TEEs as cardiology trainees in the United States.”
In addition, he said, “The 4 hours of simulator training in TEE is extra education and experience that the standard trainees didn’t get. Would 4 extra hours of standard training didactics also improve trainees’ scores?”
Noting that the fellows’ ability to perform TEE in real patients was not assessed, Szawlewicz said, “A study could be designed that evaluated TEE images from real patients to see if trainees receiving simulator training performed better, more comprehensive and efficient TEEs than standard training.”
Nevertheless, he concluded, “Four hours of simulator training appears to improve TEE knowledge and skills. This is something we would consider at our institution.”
Like Szawlewicz, Michael Spooner, MD, MBA, of Mercy One North Iowa Heart Center in Mason City, and Kathryn Bertlacher, MD, of the University of Pittsburgh Medical Center, note in a related editorial, “[D]ata are not provided about change in the learner’s behavior or performance on an actual TEE after the course, nor are there data about clinical outcomes such as patient safety or completeness of subsequent TEEs.
“This limitation, which is a limitation of most of the existing TEE simulation literature, is a high bar to cross,” they conclude. “Reaching this bar will require studies such as this to provide foundational understanding.”
Twin-Medical provided the TEE simulators. No relevant conflicts of interest were disclosed.
JAMA Cardiol. Published online January 11, 2023. Abstract, Editorial
Follow Marilynn Larkin on Twitter: @MarilynnL. For more from the heart.org | Medscape Cardiology, follow us on Twitter and Facebook.
Source: Read Full Article