Second dose of Pfizer-BioNTech COVID-19 vaccine may not benefit previously infected individuals
Researchers at the NYU Grossman School of Medicine have shown that a second dose of the Pfizer-BioNTech BNT162b2 vaccine may not offer any additional protection against coronavirus disease 2019 (COVID-19) over one dose among individuals previously infected with the causative agent severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
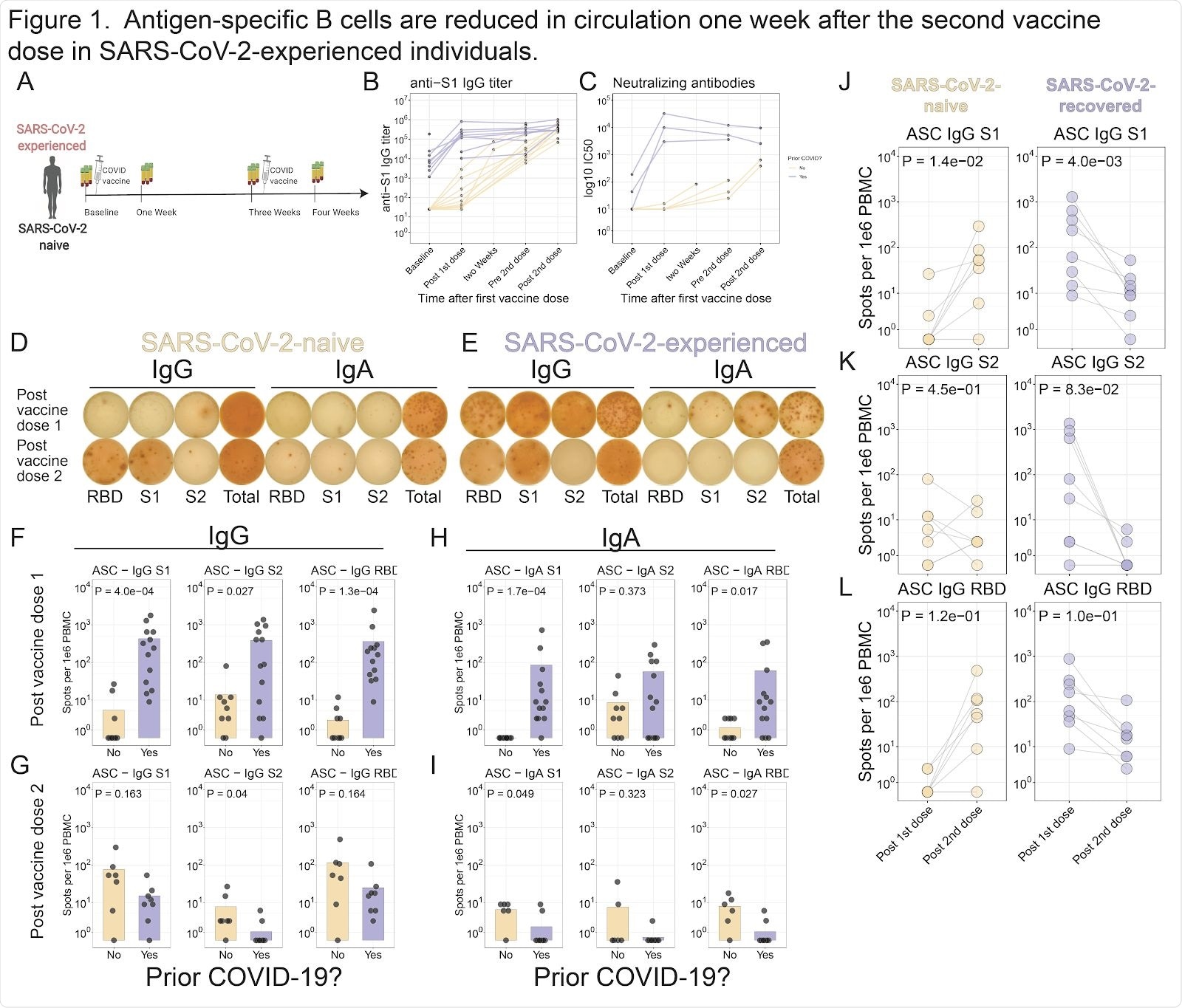
In a study evaluating immune responses to the Pfizer-BioNTech vaccine, Ramin Herati and colleagues observed robust humoral (antibody) responses following two vaccine doses among individuals without previous SARS-CoV-2 infection (SARS-CoV-2-naïve).
However, SARS-CoV-2-experienced participants had a robust humoral response to the first dose but a muted response to the second dose.
In fact, SARS-CoV-2-experienced individuals had lower circulating levels of antigen-specific antibody-secreting cells (ASCs) following the second dose than they did following the first dose.
“These data highlight an important gap in our knowledge and may have major implications for how these vaccines should be used to prevent COVID-19,” writes Herati and the team.
A pre-print version of the research paper is available on the medRxiv* server while the article undergoes peer review.
SARS-CoV-2 infection triggers important antibody responses
The SARS-COV-2 infection process is mediated by a surface structure called the spike protein, which binds to the host cell receptor angiotensin-converting enzyme 2 (ACE2) via its receptor-binding domain (RBD).
The spike protein comprises two subunits. Subunit 1 (S1) contains the RBD, which attaches to ACE2 via a receptor-binding motif (RBM) and subunit 2 (S2) enables the viral membrane to fuse with the host cell.
Following natural infection, antibodies targeting the spike RBD are thought to account for more than 90% of the neutralizing activity against SARS-CoV-2.
Research has shown that pre-existing immunity to SARS-CoV-2 is associated with protection against reinfection in humans and animals.
Recently approved vaccines are based on the spike protein
Both the Pfizer-BioNTech and Moderna vaccines that have recently been FDA-approved for emergency use against SARS-CoV-2 are mRNA-based vaccines that encode a region of the spike protein.
These novel mRNA vaccines have been considered critical to ending the COVID-19 pandemic since they were shown to induce robust humoral responses against SARS-CoV-2 and to be 94% effective at preventing disease in large-scale clinical trials.
However, efficacy trials excluded individuals with a prior diagnosis of COVID-19 and only focused on individuals without previous SARS-CoV-2 exposure.
“As a result, little is known about the immune responses in SARS-CoV-2-experienced individuals, a setting which is relevant to hundreds of millions of people worldwide,” says Herati and colleagues.
“Indeed, more studies are needed to fully understand the breadth and quality of the immune response to these vaccines.”
What did the researchers do?
The team evaluated immune responses among 32 individuals (aged 24 to 62 years) who received the Pfizer-BioNTech BNT162b2 vaccine as a two-dose regimen.
Thirteen of the participants (median age 41 years) had previously been infected with SARS-CoV-2 and the remaining 19 (median age 39 years) were SARS-CoV-2-naïve.
All participants had immune responses assessed at approximate intervals before and after each dose of the vaccine.
What did the study find?
Following the first vaccine dose, anti-S1 immunoglobulin G (IgG) titers increased 47-fold among the SARS-CoV-2-experienced individuals and 2.6-fold among the SARS-CoV-2-naïve participants.
However, following the second dose, anti-S1 IgG titers only increased 1.4-fold among the SARS-CoV-2-experienced participants, whereas they increased 13-fold among SARS-CoV-2-naïve individuals.
One week after the second dose, anti-S1 IgG titers were similar between the two groups.
“These data demonstrate rapid and robust humoral responses after vaccination in both cohorts, but there was a minimal further increase in SARS-CoV-2-experienced subjects after the second vaccine dose,” says the team.
Similarly, while antigen-specific ASC responses increased following each vaccine dose among the SARS-CoV-2-naïve subjects, fewer circulating antigen-specific ASCs were detected among SARS-CoV-2-experienced participants after the second vaccine, compared with after the first dose.
After the second dose, reductions in circulating antigen-specific ASCs were observed for S1, S2 and the RBD among SARS-CoV-2-experienced participants.
What are the implications of the study?
“Here, we observed robust antibody responses in individuals who were SARS-CoV-2-naive,” says Herati and colleagues.
“In contrast, SARS-CoV-2-experienced subjects responded strongly to the first dose of vaccine with increased antibodies and antigen-specific ASC responses, but did not respond as strongly following a second vaccine dose,” they write.
The researchers say the findings highlight the need to investigate further the impact that prior immunological experience of SARS-CoV-2 may have on responses to COVID-19 vaccines.
“Future studies may be needed to determine whether more optimal dosing regimens are needed for durable, protective immunity to infection by the SARS-CoV-2 virus,” they conclude.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Herati RS, et al. Poor antigen-specific responses to the second BNT162b2 mRNA vaccine dose in SARS-CoV-2-experienced individuals. medRxiv, 2021. doi: https://doi.org/10.1101/2021.02.07.21251311, https://www.medrxiv.org/content/10.1101/2021.02.07.21251311v1
Posted in: Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Antigen, Assay, Cell, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Enzyme, Immune Response, Immunoglobulin, in vitro, Medicine, Pandemic, Protein, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus

Written by
Sally Robertson
Sally has a Bachelor's Degree in Biomedical Sciences (B.Sc.). She is a specialist in reviewing and summarising the latest findings across all areas of medicine covered in major, high-impact, world-leading international medical journals, international press conferences and bulletins from governmental agencies and regulatory bodies. At News-Medical, Sally generates daily news features, life science articles and interview coverage.
Source: Read Full Article



