Patients reported international hydroxychloroquine shortages due to COVID-19

A new study shows that patients with rheumatic diseases across Africa, Southeast Asia, the Americas and Europe had trouble filling their prescriptions of antimalarial drugs, including hydroxychloroquine, during the 2020 global coronavirus pandemic, when antimalarials were touted as a possible COVID-19 treatment. Patients who could not access their antimalarial drugs faced worse physical and mental health outcomes as a result. Details of the research was presented at ACR Convergence, the American College of Rheumatology’s annual meeting (ABSTRACT #0007).
Systemic lupus erythematosus, also called lupus or SLE, is a chronic (long-term) disease that causes systemic inflammation which can affect multiple organs: the skin, joints, kidneys, the tissue lining the lungs (pleura), heart (pericardium) and brain. Many patients experience fatigue, weight loss and fever. Antimalarial drugs are taken regularly by most people with lupus, as well as many with rheumatoid arthritis (RA) and other rheumatic diseases.
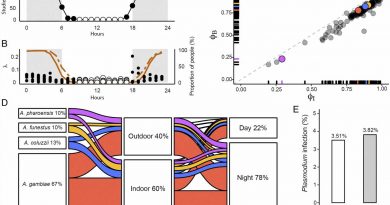
In the early weeks of the global SARS-CoV-2 (COVID-19) pandemic, two antimalarial drugs often used to treat lupus and RA, hydroxychloroquine and chloroquine, were touted to potentially prevent or treat COVID-19 infections. Both drugs were suddenly repurposed as COVID-19 treatments despite a lack of data to support this use, leading to worldwide shortages of both. A team of international researchers launched this study to assess the effects of antimalarials on COVID-19 infection and the impact of drug shortages on people with rheumatic disease.
“The COVID-19 Global Rheumatology Alliance’s Patient Experience Survey was launched in April 2020 during the early days of the pandemic, when the scientific and research communities were under extraordinary pressure to identify safe and effective treatments for SARS-CoV-2. Since hydroxychloroquine is an essential treatment for RA and lupus, reported drug shortages of antimalarials became a major concern,” says the study’s lead author, Emily Sirotich, a doctoral student at McMaster Centre for Transfusion Research in Hamilton, Ontario. and Patient Engagement Lead of the COVID-19 Global Rheumatology Alliance. “The aims of this study were to assess the prevalence and impact of drug shortages during the COVID-19 pandemic, and whether the use of antimalarials in patients with rheumatic disease was associated with a lower risk of COVID-19 infection.”
Data for the new study was collected using the COVID-19 Global Rheumatology Alliance Patient Experience Survey. The survey was distributed online through patient support organizations and social media. Both patients with rheumatic diseases and parents of pediatric patients anonymously completed the surveys with information on their rheumatic disease diagnosis, medications they take, COVID-19 status and any disease outcomes. The researchers evaluated the impact of antimalarial drug shortages on patients’ disease activity, as well as their mental health and physical health.
Of the 9,393 people who responded to the survey, 3,872 were taking antimalarial drugs and 230 said they were unable to continue taking their medications because of a lack of supply at their pharmacy. Antimalarial shortages were worse for people in Africa and Southeast Asia: 26.7% of respondents in Africa and 21.4% of respondents in Southeast Asia reported inadequate supplies at local pharmacies. Patients in the Americas (6.8%) and Europe (2.1%) also reported being unable to fill their prescriptions at their pharmacy due to lack of supply.
The study found that patients on antimalarials and those who did not take these drugs had similar rates of COVID-19 infection. A total of 28 patients with COVID-19, who were also taking antimalarials, were hospitalized. Of 519 patients diagnosed with COVID-19 in the survey, 68 reported that they were prescribed an antimalarial for their coronavirus infection. Patients who could not fill their antimalarial prescriptions experienced higher levels of disease activity and also experienced worse mental and physical health symptoms, the study found.
Source: Read Full Article