Hox genes control stem cells involved in forming and repairing bone
Genes long known to control the formation of bones before birth also control bone healing later in life, a new study found.
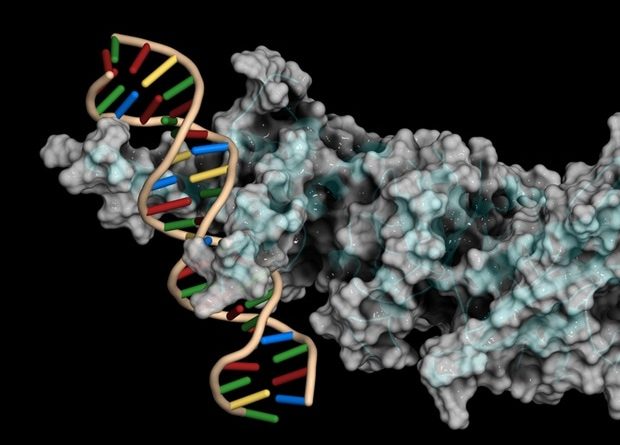
Led by researchers at NYU Langone Health, a new study pinpointed key Hox genes, specific to each location in the body, as the controllers of stem cells involved in both forming and repairing bone. HOX proteins act like the body’s “zip code,” specifying the position of limbs in the fetus by encoding instructions for transcription factors, which attach to DNA and influence the action of genes.
Such adjustments guide immature stem cells as they multiply and mature in the womb, say the study authors, to become heart muscle, nerves, bones, etc., and in the right places. Bone is among the tissues that keep pools of stem cells on hand into adulthood, ready to mature into needed replacement cells that maintain healthy tissue and heal broken bones.
Published online recently in the journal Development, the new work found that Hox genetic programs in adulthood control a bone stem cell type called periosteal stem and progenitors cells, or PSCPs. These cells play a central role in healing bones according to the womb-determined positions in which they first formed. Already known to encode the spatial code that sets the body’s formation plan, HOX genes were shown in the study to give adult stem cells from different locations the properties needed to regenerate the particular bone in which they reside.
During aging, such stem cells become depleted, the researchers say, resulting in weaker bones that are more likely to fracture and slower to heal. In an effort to counter this loss in healing, the research team demonstrated that increasing the activity of the gene that directs the building of the Hoxa10 transcription factor in the tibia, the larger of the two “shin bones,” in aging mice caused a 32.5 percent restoration of fracture repair capacity.
Our data revealed a previously unknown function for Homeobox or Hox genes as essential location-specific regulators of stem cell maturity in adulthood, with short-term local increases in their expression able to drive healing. The therapeutic promise of adult stem cells as a source of bone-making cells in healing-compromised people is massive.”
Philipp Leucht, MD, PhD, Corresponding Study Author, the Raj-Sobti-Menon Associate Professor of Orthopedic Surgery in the Department of Orthopedic Surgery at NYU Grossman School of Medicine
Bone requires attention
Omics eBook

A fundamental question in the field has been whether bone healing is driven more by stem cells in the marrow in a bone’s center, or by those known to pool in the nearby periosteum, the outer bone layer made of up tough connective tissue and cell-filled areas. Both stem cell types have the capacity to mature into osteoblasts, the cells that lay down new bone in response to a fracture, but the current study argues that stem cells in the periosteum, the PSPCs, are the important contributors to bone repair.
The study result builds on the understanding that, to keep stem cells pools on hand, they must get signals to continually divide and multiply without maturing, maintaining their “stemness” until needed. The body regulates bone repair by controlling the degree to which stem cells stay immature, with the most primitive cells playing the largest role in healing due to their flexibility and ability to quickly multiply.
In the current study, the researchers found that Hox deficiency leads to an increase in the stem cells’ propensity to differentiate into mature bone cell types. Conversely, when the team increased Hoxa10 expression in tibia stem and progenitor cells, it reprogrammed them into a more stem cell-like state, a needed step if they are to become new bone-making cells as part of healing.
Specifically, say the authors, PSPCs exist as a mixed stem cell population that includes those with the most stemness, naive periosteal stem cells (PSCs), alongside more mature periosteal progenitor 1 and 2 (PP1 and PP2) cells. The current study authors found that Hoxa10 expression was most abundant in PSCs and was significantly reduced as cells progressed along the lineage hierarchy to PP1 and PP2. Experiments that increased the activity of the Hox genes in these more mature progenitors brought about a threefold increase of PSCs as cells were reprogrammed into a more primitive stem cell identity.
“PSPCs have distinguishing characteristics that form the basis for future cell-based therapies, including their greater tendency to naturally regenerate bone than many related stem cell groups,” said co-corresponding lead author Kevin Leclerc, a postdoctoral scholar in Dr. Leucht’s lab. “By modifying Hox activity in these cells, we can help them regenerate bone more effectively in individuals with deficient bone-healing capacity.”
NYU Langone
Leclerc, K., et al. (2023). Hox genes are critical regulators of periosteal stem cell identity. Development. doi.org/10.1242/dev.201391.
Posted in: Cell Biology | Genomics
Tags: Aging, Bone, Cancer, Cell, DNA, Fracture, Gene, Genes, Genetic, Heart, Medicine, Muscle, Orthopedic, Progenitor Cells, Research, Stem Cells, Surgery, Transcription, Transcription Factors, Womb
Source: Read Full Article