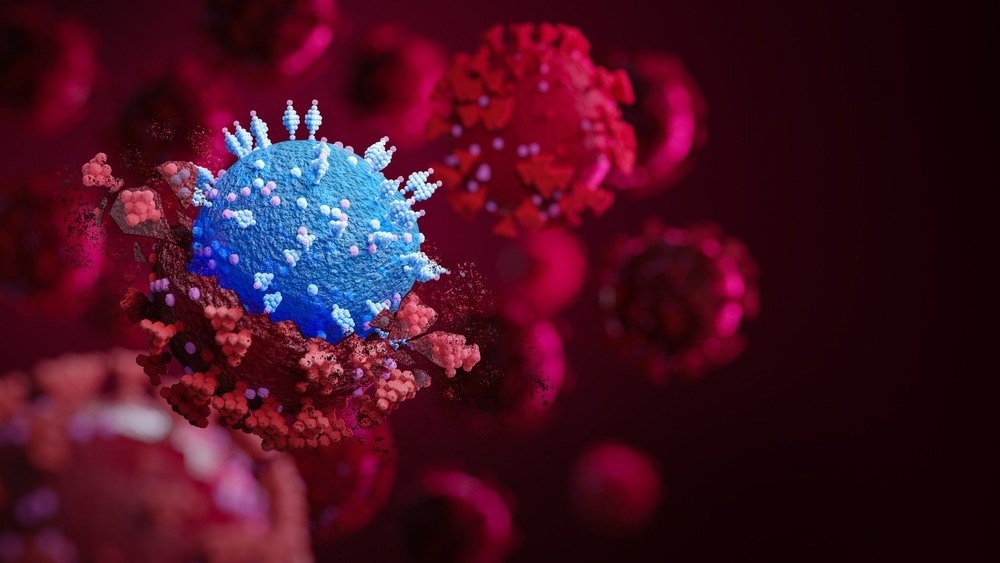
How do mutations in emergent SARS-CoV-2 Omicron variants affect viral function, human immunity, and recognition by therapeutic antibodies?
In a recent study posted to bioRxiv*, researchers explored how mutations in emergent severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants affect viral function, human immunity, and recognition by therapeutic antibodies.
Background
Several Omicron lineages are currently co-circulating globally. Many independently acquired similar/identical amino acid substitutions at critical antigenic sites in the spike protein's receptor-binding (RBD) and N-terminal (NTD) domains. The Omicron BA.2.75 variant harbors several additional mutations relative to BA.2. XBB.1 is a recombinant lineage derived from BA.2.75 and BJ.1, which, too, has additional modifications compared to BA.2.
The study and findings
In the present study, researchers examined the impact of mutations in SARS-CoV-2 BA.2.75, BQ.1.1, and XBB.1 variants on viral functional characteristics, humoral responses, immune memory, and therapeutic antibody recognition. First, they used biolayer interferometry (BLI) to evaluate the binding affinity and kinetics of human angiotensin-converting enzyme 2 (hACE2) to variant RBDs.
BLI revealed a similar binding affinity for BA.5 and BQ.1.1 RBDs, suggesting that additional mutations of BQ.1.1 did not impact hACE2 engagement. It also showed a higher binding affinity of BA.2.75 RBD relative to BA.2. XBB.1 RBD had a similar affinity as Wuhan-Hu-1 (Wu) RBD. Surface plasmon resonance (SPR) revealed results comparable to BLI. The team observed reduced and slower fusogenicity for BA.1, BA.2, and BA.5 spikes relative to the Delta spike.
By contrast, spikes of XBB.1, BA.2.75.2, and BQ.1.1 variants promoted fusion more efficiently than earlier Omicron lineages. Next, they investigated the preferred cellular entry route of emergent variants since prior studies reported that Omicron variants (BA.1, BA.2, and BA.5) preferentially used the cathepsin-mediated endosomal route as opposed to membrane fusion, mediated by transmembrane protease, serine 2 (TMRPSS2).
TMPRSS2 inhibitors blocked the entry of Delta pseudoviruses in VeroE6-TMPRSS2 cells, with limited effects on any Omicron variant. On the other hand, the cathepsin inhibitor (E64d) blocked the entry of BA1, BA.2, and BA.5 pseudoviruses without affecting the entry of Delta, BQ.1.1, XBB.1, or BA.2.75.2 pseudoviruses. Next, the team assessed the binding affinity and kinetics of S309, a monoclonal antibody (mAb), to variant RBDs using SPR.
Antibodies eBook
The binding affinity of the mAb to variant RBDs decreased approximately 100-fold relative to Wu RBD. In addition, sotrovimab (an S309 derivative) showed efficient cross-reactivity to cell surface-expressed spike trimers of XBB.1 and BQ.1.1 variants. Nonetheless, neutralization potency was variable, with about 6.5- and 94-fold loss against XBB.1 and BQ.1.1, respectively, relative to Wu.
Moreover, sotrovimab promoted antibody-dependent cytotoxicity (ADCC) of cells expressing spikes of BA.2, XBB.1, or BQ.1.1. Further, K18/hACE2 mice received S309 as prophylaxis a day before SARS-CoV-2 BQ.1.1 challenge. The mAb protected animals from body weight loss and reduced infectious virus titers and viral RNA in the lung. These findings showed that S309 could protect mice, despite the loss of in vitro neutralization potency against BQ.1.1.
Next, the team analyzed plasma obtained after vaccination or breakthrough infection from eight cohorts of individuals for pseudovirus-neutralizing activity. Wu/BA.1 or Wu/BA.5 bivalent mRNA vaccines induced higher neutralizing antibody (nAb) titers against BA.1 or BA.5 pseudoviruses. Individuals who received bivalent vaccines showed detectable neutralization against vaccine-mismatched pseudoviruses (XBB.1, BQ.1.1, and BA.2.75.2), regardless of prior infection status.
Additional experiments indicated that plasma antibodies eliciting fragment-crystallizable (Fc) effector functions varied among individuals but were broadly reactive against Omicron variants. The researchers compared memory B cells (MBCs) among four (of the eight) cohorts by enumerating the frequency of Wu and Omicron RBD-specific MBCs and Wu/Omicron cross-reactive MBCs.
Individuals vaccinated with the Wu spike mRNA vaccine had the highest Wu RBD-specific MBCs and the lowest cross-reactive MBCs. Most specific MBCs were cross-reactive to Wu and Omicron RBDs. Individuals vaccinated with the Wu/BA.5 bivalent vaccine with an Omicron breakthrough infection had relatively few Omicron-specific RBDs, although cross-reactive MBCs were highly enriched.
Most cross-reactive and fewer Omicron RBD-specific MBCs recognized BQ.1.1 RBD, regardless of vaccination or infection status. Finally, the team noted that Wu/BA.1 mRNA booster vaccine failed to induce Omicron-specific MBCs in infection-naïve individuals or those with an Omicron breakthrough infection. These findings suggested that two Omicron exposures were insufficient to overcome the immune imprinting caused by multiple exposures to the Wu spike but can enrich cross-reactive MBCs.
Conclusions
In sum, the research team demonstrated that emergent SARS-CoV-2 Omicron variants exhibit unprecedented levels of immune evasion. BA.2.75.2 and BQ.1.1 variants had a high binding affinity for ACE2, while XBB.1 had a lower binding affinity. Although XBB.1 showed the highest level of immune evasion, its reduced ACE2 affinity might explain the hindered spread. Together, the results illustrated the complex interplay of ACE2 affinity, fusogenicity, and immune evasion in SARS-CoV-2 evolution.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Addetia, A. et al. (2023) "Therapeutic and vaccine-induced cross-reactive antibodies with effector function against emerging Omicron variants". bioRxiv. doi: 10.1101/2023.01.17.523798. https://www.biorxiv.org/content/10.1101/2023.01.17.523798v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, ADCC, Amino Acid, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, binding affinity, Cell, Coronavirus, Coronavirus Disease COVID-19, Cytotoxicity, Enzyme, Evolution, Frequency, immunity, in vitro, Membrane, Monoclonal Antibody, Omicron, Prophylaxis, Protein, Pseudovirus, Receptor, Research, Respiratory, RNA, SARS, SARS-CoV-2, Serine, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sotrovimab, Spike Protein, Syndrome, Vaccine, Virus, Weight Loss

Written by
Tarun Sai Lomte
Tarun is a writer based in Hyderabad, India. He has a Master’s degree in Biotechnology from the University of Hyderabad and is enthusiastic about scientific research. He enjoys reading research papers and literature reviews and is passionate about writing.
Source: Read Full Article



