Acidity of expiratory aerosols influences infectivity of SARS-CoV-2
Enveloped viruses can be inactivated by exposure to acids, such as within aerosols in the atmosphere. A new study posted to the medRxiv* preprint server provides insight on the potentially significant impact of aerosol pH on the transmission of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Study: Acidity of Expiratory Aerosols Controls the Infectivity of Airborne Influenza Virus And SARS-Cov-2. Image Credit: Aranami / Shutterstock.com
Introduction
Respiratory viral infections are among the most common human illnesses. For example, the influenza virus is responsible for about 400,000 deaths each year worldwide, while the ongoing coronavirus disease 2019 (COVID-19) pandemic has caused over six million deaths in the two years since its inception. Virus transmission is therefore a prime target of prevention strategies and other interventions intended to contain outbreaks.
Many experts have indicated that respiratory aerosols formed during expiration are important in the spread of both influenza and SARS-CoV-2. Thus, the rapid inactivation of these pathogens is an important step in restricting their transmission.
However, beyond temperature and humidity, there is limited data available on the relationship between aerosol acidity and the inactivation of these viruses. The pH of the aerosol depends both on the composition of the particles in the aerosol and of the ambient air.
Particles in outdoor air are highly acidic, with the pH plunging as low as -1. The more volatile the acid or base in the aerosol, such as nitric acid and ammonia, the greater the effect on the pH, as these chemicals rapidly condense on aerosol particles. Notably, the presence of strong organic acids like vinegar or formic acid is of minor significance with respect to aerosol pH.
Indoors, these volatile acids are at lower concentrations, as they condense rapidly on both particles and surfaces. Nitric acid and ammonia levels in indoor air are therefore 0.1-0.5 and three to 30 times that in outdoor air, while organic acids are also elevated.
The use of humidification, ventilation, and air conditioning (HVAC) systems is another major factor that can impact air composition. Expiratory aerosols are rich in ammonia and carbon dioxide, along with a considerable amount of aerosol particles including ions, proteins, and surfactants.
The current study explores how aerosol acidity is related to the inactivation of the influenza A virus (IAV), SARS-CoV-2, and the seasonal human coronavirus HCoV-229E (229E) indoors.
Study findings
Inactivation times were found to decrease from a matter of days to seconds, covering five orders of magnitude, as the pH was reduced from 6 to 4. The concentration of the synthetic lung fluid (SLF) in which the viruses were immersed in one set of samples did affect the inactivation time, with the extrapolated data showing an increase in inactivation time by up to a factor of 56 when SLF was enriched 18 times.
Concentrated SLF was thus protective against IAV inactivation, especially around the pH optimal for IAV fusion, but less so against the coronaviruses, which remained stable down to pH 3. Beyond this point, when inactivation required 24 hours at a pH of 2, the inactivation times declined rapidly to less than ten seconds for SARS-CoV-2. However, the minimum inactivation time remained above two hours for HCoV-229E.
This difference is hypothesized to be due to the difference in the way these viruses enter the host cells. IAV uses a hemagglutinin antigen, which changes conformation during endosomal entry and relies on acidification. The irreversible nature of this conformational shift means that once it occurs outside the cell at an acidic pH, the virus is no longer able to bind to the host cell receptor, thereby leading to its inactivation.
Comparatively, the spike protein of coronaviruses, which is responsible for cell entry, does not undergo fusion-mediating conformational shifts due to acidification but rather because of host protease activity. Still, the two coronaviruses here showed different activity patterns at a pH below 3.
When the individual micron-sized SLF and nasal mucus particles were studied for their thermodynamic behavioral and kinetic properties, differences were found in the salt composition, which affects deliquescence, and water uptake or loss. The differences in water loss at each stage may be due to variations in the mode of salt crystal formation within and at the surface of the droplet.
The limit on the diffusion of ions in the SLF and nasal mucosa differs from the universally fast diffusion of water in both media. The latter rules out the formation of semisolid phases that would prevent diffusion, as suggested by some earlier studies.
The scientists combined virus properties with aerosol thermodynamics and kinetics data to build a biophysical model called the Respiratory Aerosol Model (ResAM). This was intended to simulate changes in the composition and pH of the expiratory particle during expiration, and determine how this changed viral infectivity.
When considering changes in relative humidity with the ion and water diffusivities, the model was able to predict the mass fraction of solutes among both deliquescence and efflorescence. This accuracy is dependent on the inclusion of kinetic effects.
As the pH reduces, a particle with a diameter of two microns will undergo rapid water loss, along with the concentration of organic compounds and salts, until the salt sodium chloride undergoes effloresces. Nitric acid in indoor air quickly enters the particle, thus causing a sharp drop in its pH.
The room air, which has a pH of about 6.6 due to high carbon dioxide and ammonia levels, accepts nitric acid into its aerosol particles. This reduces the pH to 5 within seconds, thereby pulling the basic ammonia into the particle. The pH was found to further decline to 3.7 slowly as more nitric acid is absorbed into the particle.
If only carbon dioxide is measured, the pH of the exhaled particle would be expected to rise, which emphasizes the need to measure trace gases in determining the actual pH of indoor air aerosol particles. In such acidic conditions of expiratory aerosol, IAV would be inactivated within two minutes; however, the coronaviruses remain infectious.
Particle size also correlates positively with inactivation times. This is because the larger the particle, the longer the time needed to reach an acidic pH as a result of the need for ions and molecules to diffuse over a longer pathway in air and liquid phases. Within 2 minutes, 99% of IAV particles below a radius of one micron, which is typical of expiratory particles, undergo inactivation, whereas those larger than one millimeter remain active for up to 5 days.
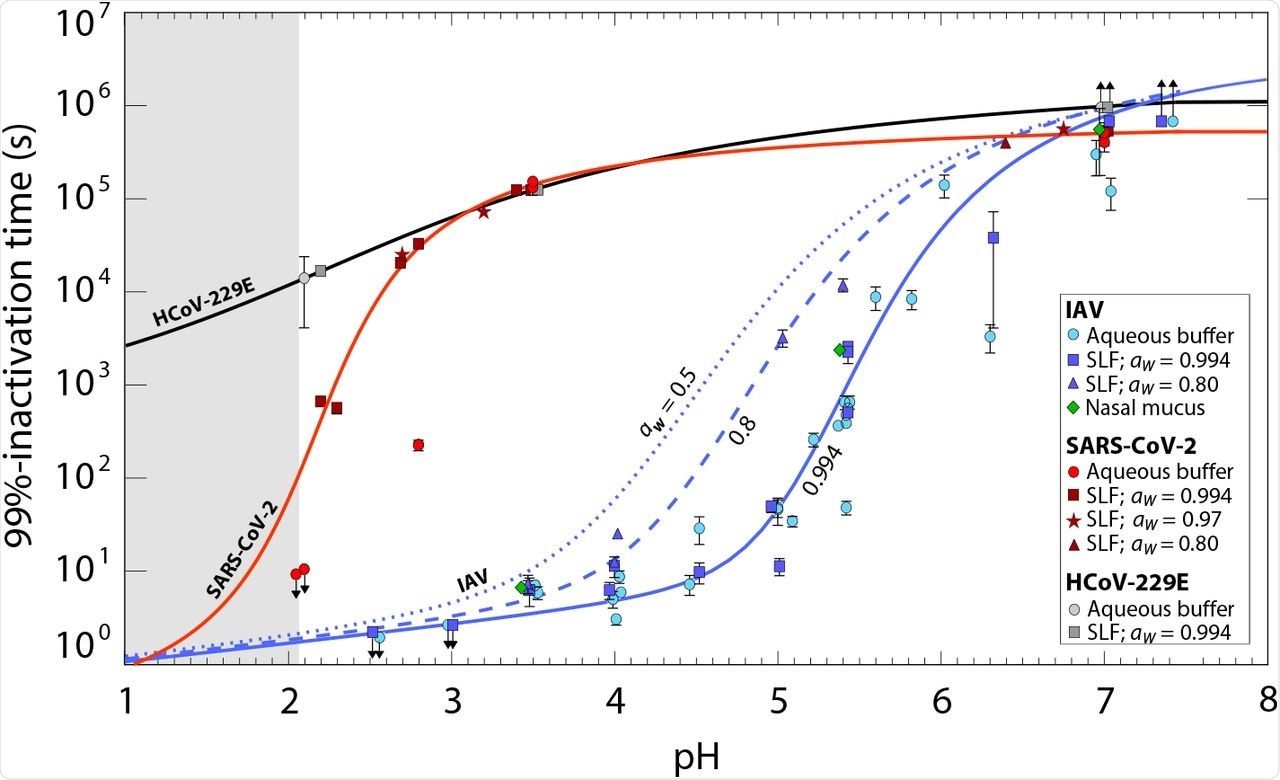
Time required for 99% titer reduction of influenza A virus (IAV), SARS-CoV-2 and human coronavirus HCoV-229E measured in various bulk media (> 10 µl) at 22°C. Data points represent inactivation times in aqueous citric acid/Na2HPO4 buffer, synthetic lung fluid (SLF) or nasal mucus with pH between 7.4 and 2. SLF concentrations correspond to water activity aw = 0.994 (1 × SLF; squares), aw = 0.97 (5 × SLF; stars) and aw = 0.8 (18 × SLF; triangles); buffer (circles) and nasal mucus (diamonds) correspond to aw ∼ 0.99. Each experimental condition was tested in replicate with error bars indicating 95% confidence intervals. While IAV displays a pronounced reduction in infectivity around pH 5, SARS-CoV-2 develops a similar reduction only close to pH 2, and HCoV-229E is largely pH-insensitive. Solid lines are arctan fits to SLF data with aw = 0.994 (blue: IAV; red: SARS-CoV-2; black: HCoV-229E). The dashed line is an arctan fit to the SLF data with aw = 0.80. The dotted line is an extrapolation to aw = 0.5 (24 × SLF). Upward arrows indicate an insignificant change in titer over the course of the experiment, and downward arrows indicate inactivation below the level of detection at all measured times. The fitted curves below pH 2 (grey shaded area) are extrapolated with high uncertainty. Examples of measured inactivation curves are shown in Fig. S1. The arctan fit equations, which are also used for the model simulations, are given by Eqns. S28, S29, and S30.
Thus, a rise in particle size is closely proportional to IAV inactivation time when indoor conditions are considered, while at all sizes, SARS-CoV-2 remains active for much longer. With acidification of indoor air, both IAV and SARS-CoV-2 are much more quickly inactivated, if only the acidic molecules of the aerosol are volatile enough that they quickly pass from being in the gaseous to condensed phase. Additionally, gaseous acid molecules must be strong enough to compensate for the buffering effect of particles in the particle matrix.
The introduction of larger particles caused the pH to decline rapidly and significantly as compared to when volatile organic acids like acetic acid were introduced into the cells. SARS-CoV-2 inactivation occurred four to five orders faster in this air as compared to typical room air.
Purifying air reduces trace gases, such that strong organic acids that are already two times lower indoors as compared to outdoors drop in concentration by 10-80 times. This causes the aerosol pH to rise above that of indoor air, thereby becoming neutral or even a little basic.
As a result, air purification is expected to enhance virus persistence, especially for IAV.”
Conclusions
The results of the current study were demonstrated by modeling. The addition of 50 parts per billion (ppb) of nitric acid fails to improve the inactivation time of HCoV-229E but may reduce transmission risks of IAV and SARS-CoV-2 by 20 and 800 times.
Conversely, increasing ventilation from two air changes per hour to ten per hour reduces the concentration of SARS-CoV-2 by five times, while it does not affect the already rapid inactivation of IAV.
Normal air purification systems reduce important trace gases like nitric acid; however, this is more important when the air filters contain activated carbon, which enhances acid removal. This could increase the risk of IAV spread significantly in such buildings as compared to those that use outdoor air without filtration.
Here we demonstrate that a significant reduction in transmission risk can be achieved by air enrichment with HNO3 levels that correspond to less than 10% of the legal exposure thresholds.”
While these fall below human exposure thresholds, their effects on the microbiome and immune response of the respiratory tract remain to be known in future studies, as well as the effects of other respiratory matrices.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Luo, B., Schaub, A., Glas, I., et al. (2022). Acidity of Expiratory Aerosols Controls the Infectivity of Airborne Influenza Virus And SARS-Cov-2. medRxiv. doi:10.1101/2022.03.14.22272134. https://www.medrxiv.org/content/10.1101/2022.03.14.22272134v1.
Posted in: Microbiology | Medical Science News | Medical Research News | Disease/Infection News
Tags: Antigen, Cell, Chemicals, Coronavirus, Coronavirus Disease COVID-19, covid-19, Immune Response, Influenza, Ion, Microbiome, Pandemic, Particle Size, pH, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article