A review of natural immunity, vaccines, and variants in SARS-CoV-2 reinfection
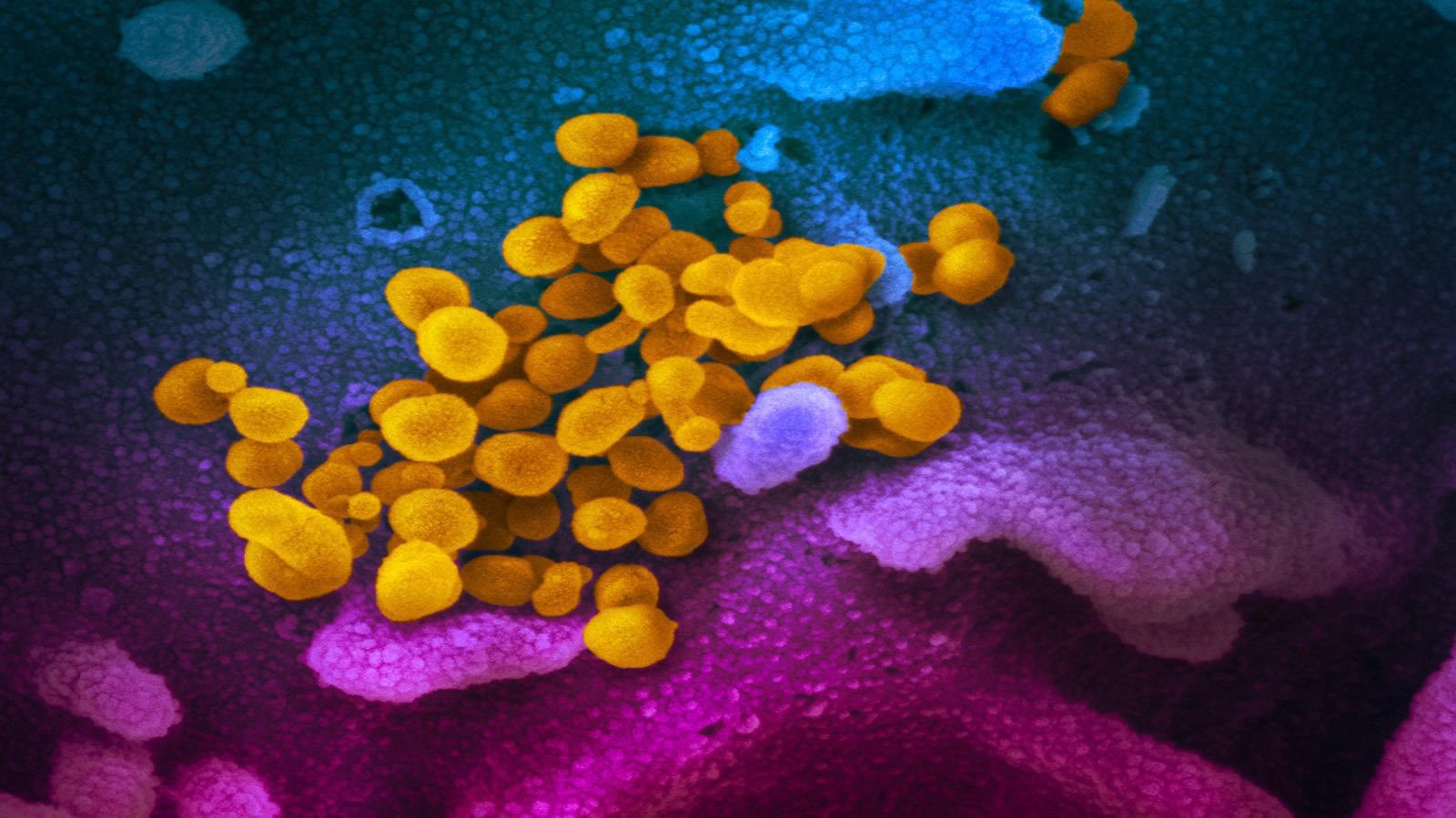
The coronavirus disease 2019 (COVID-19) pandemic is an ongoing global health issue caused by the novel coronavirus severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2).
Many rigorous studies have been conducted to understand the pathogenesis and transmissibility of SARS-CoV-2. Despite all these efforts, many areas are still unexplored, such as SARS-CoV-2 reinfection and reactivation.
More comprehensive studies are required to evaluate the possibility of reinfection and its potential risk factors.
Literature review on COVID-19 reinfection
In a literature review article published in the Journal of Community Hospital Internal Medicine Perspectives, authors from the US performed a thorough investigation of previous studies and case reports of SARS-CoV-2 reinfection. This review discusses the role of natural immunity, vaccines, and SARS-CoV-2 variants in reinfection.
Definition of reinfection
According to the Centers for Disease Control (CDC), reinfection is defined as "an infection in an individual with two different viral strains within ≥45 days in highly suspicious cases of COVID-19 disease or ≥90 days in asymptomatic cases or cases with low suspicion".
In addition, some studies define reinfection as having negative tests in between two positive SARS-CoV-2 reverse transcription-polymerase chain reaction (RT-PCR) tests besides the genotypic variation.
This review considered reinfection in individuals tested for SARS-CoV-2 using RT-PCR during the first pandemic wave before June 2020 and followed the study group from September to December 2020 to evaluate SARS-CoV-2 contraction.
A study by Tillett et al. discussed the first case of reinfection in the US in a 25-year-old man whose two nasopharyngeal RT-PCR reports within the gap of 2 months revealed genetically different variants of SARS-CoV-2.
Another study by Hall et al. found that the previous history of SARS-CoV-2 infection can lower the risk of reinfection by 83%, and its protective effect may last up to 5 months.
Likewise, many reports have been published on the properties and duration of immunity that play a vital role in reinfection.
Post-acute sequelae of SARS-CoV-2 infection
COVID-19 patients experience multiple presentations of inflammatory damage and immunologic dysregulation 4 weeks from the onset of infection known as post-acute sequelae of SARS-CoV-2 infection (PASC) and are always perceived as reinfection. Therefore, understanding the difference between PASC and reinfection is key to managing COVID-19.
Reinfection and vaccination
The US Food and Drug Administration (USFDA) has approved several vaccines targeting the spike glycoprotein of SARS-CoV-2. A two-dose vaccination regimen with Pfizer/BioNTech and Moderna/National Institute of Allergy and Infectious Diseases (NIAID) is about 95% effective in preventing symptomatic COVID-19, and a single-dose regimen with Johnson and Johnson Janssen Biotech vaccine is 65.5% effective.
Other vaccines such as Covaxin, AstraZeneca/Oxford, Sputnik V vaccines with the efficacy of 78%, 70.4%, and 91.6%, respectively, have been approved in the rest of the world. However, some vaccines developed in China and others are still in different phases of clinical trials.
From December 2020, new variants of concern, including SARS-CoV-2 B.1.1.7 (Alpha), B.1.351 (Beta), B.1.617.2 (Delta) P.1. (Gamma), B.1.427 and B.1.429 (Epsilon), and now B.1.1.529 (Nu), have emerged, all with mutations in the receptor-binding domain of the spike protein. Thus, the emergence of various SARS-CoV-2 variants leads to uncertainty about the effectiveness of vaccines.
Antibodies and reinfection
In the majority of COVID-19 patients, the levels of immunoglobulin G (IgG) and IgM rise after symptom onset. However, several infected patients do not develop any antibodies for some unknown reasons. The level of antibodies in severe COVID-19 patients is more robust than those found in patients with mild or asymptomatic infection. The antibody levels begin to decrease within 60 to 90 days after the infection onset. According to some reports, immunity from these antibodies lasts long from 7 to 12 months. A study by To et al. found that reinfection can be determined by the increased immune response with IgG neutralizing antibodies and lack of IgM antibodies.
Conclusions
In the review, it was concluded that antibody responses determine SARS-CoV-2 immunity and the longevity of reinfection. In order to better understand this concept of reinfection, it would be helpful to determine the role of vaccines in reinfection with different strains. The authors suggest more comprehensive studies on patients' viral loads, viral genotypes, antibodies, and immune status to confirm true reinfection. The potential for reinfection or reactivation must be assessed in patients with asymptomatic infections.
- Bao Y. Sciscent, Caroline D. Eisele, Lisa Ho, Steven D. King, Rohit Jain & Reshma R. Golamari (2021) COVID-19 reinfection: the role of natural immunity, vaccines, and variants, Journal of Community Hospital Internal Medicine Perspectives, 11:6, 733-739, https://doi.org/10.1080/20009666.2021.1974665, https://www.tandfonline.com/doi/full/10.1080/20009666.2021.1974665
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Allergy, Antibodies, Antibody, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Food, Global Health, Glycoprotein, Hospital, Immune Response, immunity, Immunoglobulin, Infectious Diseases, Medicine, Nasopharyngeal, Pandemic, Polymerase, Polymerase Chain Reaction, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Transcription, Vaccine

Written by
Susha Cheriyedath
Susha has a Bachelor of Science (B.Sc.) degree in Chemistry and Master of Science (M.Sc) degree in Biochemistry from the University of Calicut, India. She always had a keen interest in medical and health science. As part of her masters degree, she specialized in Biochemistry, with an emphasis on Microbiology, Physiology, Biotechnology, and Nutrition. In her spare time, she loves to cook up a storm in the kitchen with her super-messy baking experiments.
Source: Read Full Article



