Pregnancy may increase the risk of a debilitating hip condition called transient osteoporosis
A review published in the journal Medicine investigates the link between transient osteoporosis of the hip (TOH) and pregnancy, focusing on diagnosis, treatment, and potential contributing factors.
Lead author Dr. Athanasios Galanis MD, Ph.D., of the Department of Orthopaedic Surgery, National & Kapodistrian University of Athens, KAT General Hospital, Greece, says, “TOH’s rare occurrence is global, particularly during pregnancy and lactation. The unclear connection between pregnancy and this condition prompts an overview of current knowledge on its causes, management, and therapy. Despite classification and treatment challenges, our review aims to equip obstetricians, gynecologists, and orthopedic surgeons with updated insights to handle pregnancy-associated TOH.”
This research intends to elevate awareness about TOH’s potential link to pregnancy, emphasizing the need for further exploration into the risk factors influencing its development in pregnant women.
In comparison to typical pregnancy-related changes, how significant are the hip pain and loss of bone mineral density linked to TOH in pregnant women?
The study discovered data suggesting that TOH-associated bone mineral density (BMD) loss in pregnant women is substantial and differs notably from the normal changes witnessed in a typical pregnancy. Studies comparing BMD alterations between pregnant women with TOH and those experiencing standard pregnancy-related changes showcased marked distinctions.
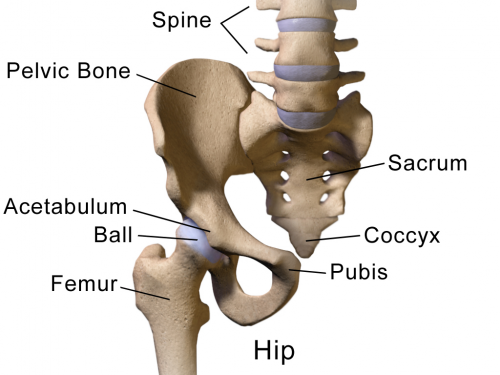
The authors noted that women who experience TOH encountered a sharper drop in bone strength compared to the usual changes seen in pregnancy. Just two weeks after giving birth, there was a notable reduction in bone strength by around 1.8% in the lower back, 3.2% in the hip, and 2.4% in the entire body. This decrease happened faster and more significantly than the minor changes expected in a normal pregnancy. Additionally, the bone strength in the forearm was also recorded to decrease during TOH, which is different from what happens in a regular pregnancy.
Likewise, hip pain associated with TOH was recorded to be considerably more acute and sudden compared to the usual discomfort experienced during pregnancy. Pregnant women with TOH reported intense groin, anterior thigh, and buttock pain, often affecting one or both hips. The severity and abruptness of this pain set TOH apart from the more common musculoskeletal discomfort experienced during gestation, necessitating prompt diagnosis and appropriate management strategies.
Is it possible to lower the risks or effects of TOH diagnosis and treatment during pregnancy on delivery and postpartum recovery?
Early diagnosis and tailored treatment of TOH during pregnancy holds potential to mitigate risks and alleviate effects on delivery and postpartum recovery. Detecting TOH through MRI, particularly during acute persistent pain episodes can enable timely intervention, thus reducing the likelihood of complications or misdiagnosis as avascular necrosis (AVN) of the hip.
Utilizing non-weight-bearing approaches, employing crutches, physiotherapy, and mild analgesics during pregnancy can be strategies to manage TOH and minimize microfractures. Further, in terms of the usage of anticoagulants like low-molecular-weight heparin, although short-term usage might not significantly increase fracture risk, long-term use should be carefully evaluated.
Moreover, distinguishing TOH from other hip pathologies via MRI allows for precise and targeted treatments. While specific medications like bisphosphonates are contraindicated during pregnancy due to fetal risks, certain safe alternatives, like calcitonin and calcium supplements can be cautiously administered. Such interventions could not only alleviate symptoms but could potentially shorten the duration of TOH and subsequent recovery time.
Dr. Galanis concludes, “We advocate for prompt MRI diagnosis in pregnant women with hip pain, advising conservative treatments and cautious use of medications. Our call for more research underscores the lack of standardized approaches for managing TOH in pregnancies, aiming for improved clinical strategies.”
Source: Read Full Article



