Gene linked to a rare neurological disorder regulates key enzyme in Alzheimer’s
A gene that can become mutated and cause a rare balance disorder also regulates the behavior of an enzyme that increases the risk for Alzheimer’s disease (AD), according to a new study by researchers at Massachusetts General Hospital (MGH) to be published in the journal Cell on August 22, 2019. This discovery may help to identify new targets for experimental medications designed to delay or stop the onset of AD.
In 2008, neuroscientist Rudolph E. Tanzi, Ph.D., director of the Genetics and Aging Research Unit and co-director of the McCance Center for Brain Health at MGH, and his colleagues identified several genes that are closely associated with AD. They include ATXN1, which carries the genetic code for producing a protein called ataxin-1. At the time, it was already known that a variation known as a “gain of function” mutation in ATXN1 causes a condition called spinocerebellar ataxia type 1 (SCA1), which afflicts one to two people per 100,000 worldwide. SCA1 leads to loss of coordination and balance, among other symptoms, which can include cognitive problems such as learning and memory difficulties.
However, the ATXN1 mutation that causes SCA1 is not associated with AD, and the role ataxin-1 might play in the disease remained unknown. “So the big question facing us was, How does a gene involved in a balance disorder somehow increase the risk for Alzheimer’s disease?” says Tanzi, senior author of the Cell paper.
The answer to that question eventually came by posing another. “We asked whether loss of ataxin-1 function could lead to Alzheimer’s disease,” says MGH neuroscientist Jaehong Suh, Ph.D. Suh supervised a team that crossbred mice that were specially bred to have the ATXN1 gene deleted, causing them to lack ataxin-1, with a second group of mice that had been bred to have AD (AD mice). These pairings produced offspring that were missing ataxin-1, which in turn made their levels of an enzyme called beta-secretase 1 (BACE1) to rise dramatically.
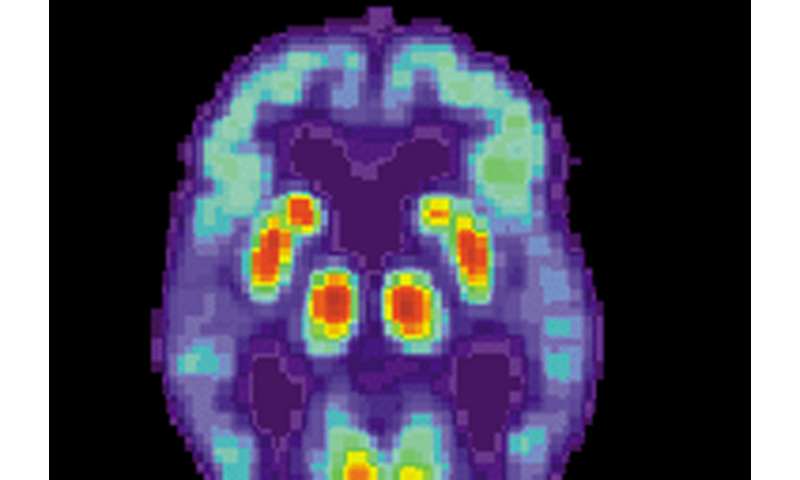
BACE1 plays an essential role in the formation of amyloid plaques, which are clusters of damaged nerve cells and other proteins in the brain that are one of the hallmarks of AD. To be sure, mice lacking ataxin-1 had significantly greater deposits of amyloid plaque than the AD mice. They also had higher levels of inflamed brain tissue, formed fewer new neurons in regions associated with memory and learning, and had impaired axons, which are fibers that carry signals between neurons.
“The idea that the same protein will cause one neurodegenerative disease in a ‘gain’ situation, and cause vulnerability to another neurodegenerative disease in a ‘loss’ situation, is fascinating,” says neurogeneticist Huda Y. Zoghbi, MD, a professor at Baylor College of Medicine, director of the Jan and Dan Duncan Neurological Research Institute in Houston, and a coauthor of the Cell study.
Source: Read Full Article



