Brain tumors occur often in kids with common genetic syndrome
The frequency of brain tumors has been underestimated in children with the common genetic syndrome neurofibromatosis type 1 (NF1), according to a new study. This disorder is characterized by birthmarks on the skin and benign nerve tumors that develop in or on the skin. Brain tumors also are known to occur in children and adults with NF1.
Neurologists have estimated that only 15 to 20 percent of kids with NF1 develop brain tumors. Of these brain tumors, the vast majority are located within the optic nerve or the brainstem. However, a recent study of brain scans performed on children with NF1 at Washington University School of Medicine in St. Louis found that the frequency of brain tumors in this population was more than three times higher. These previously under-recognized brain tumors can cause neurologic problems that require treatment.
The findings, available online in the journal Neurology: Clinical Practice, suggest that brain tumors may be a more significant problem for children with NF1 than previously appreciated.
“I’m not delivering the message anymore that brain tumors are rare in NF1,” said senior author David H. Gutmann, MD, PhD, the Donald O. Schnuck Family Professor of Neurology and director of the Washington University Neurofibromatosis Center. “This study has changed how I decide which children need more surveillance and when to let the neuro-oncologists know that we may have a problem.”
NF1 affects about one in every 3,000 people. It can affect almost any organ system, causing a wide variety of features, also including bone deformities, learning and attention deficits, autism, vision loss and cancer.
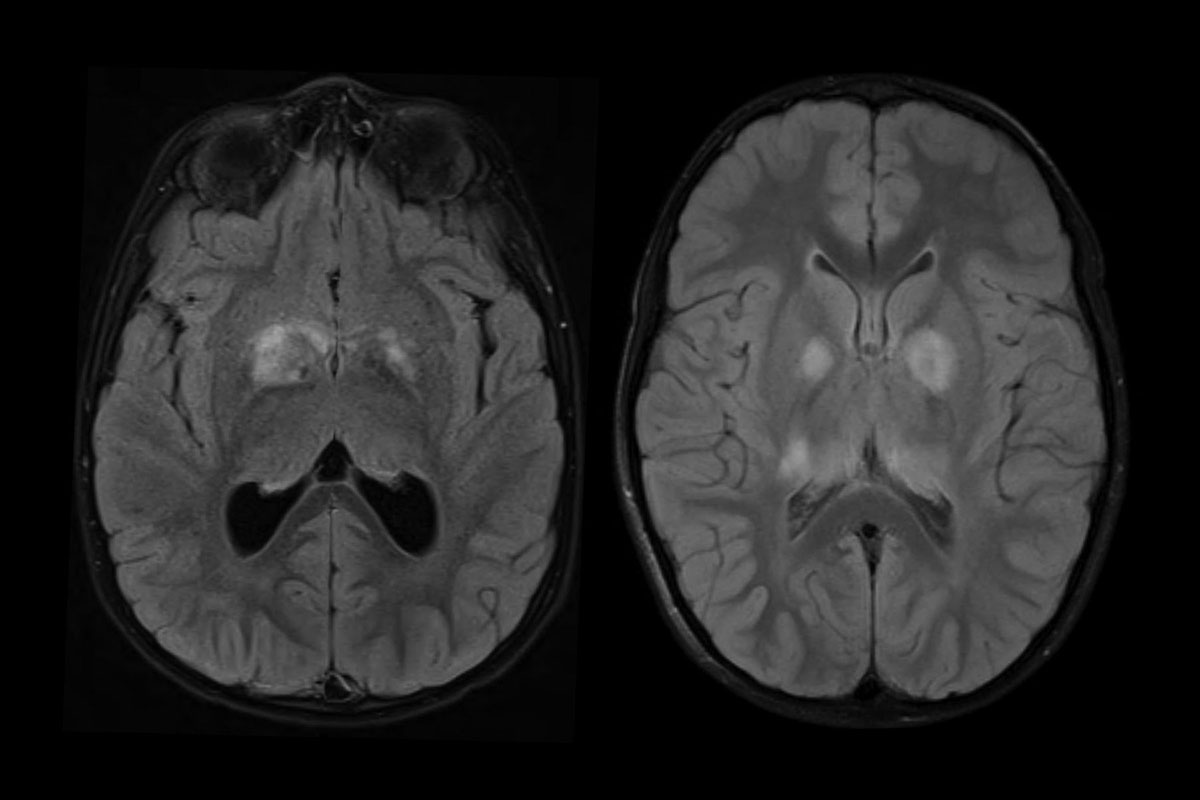
Brain MRI scans of children with NF1 characteristically show bright spots that are absent in the scans of unaffected children. Unlike tumors, they are generally thought to disappear in teenage years. Since brain tumors can be confused with harmless bright spots, it has never been clear whether finding these abnormalities via MRI should be a cause for concern.
Robert C. McKinstry, MD, PhD, the William R. Orthwein Jr. and Laura Rand Orthwein Professor of Radiology and Pediatrics, and Manu Goyal, MD, an assistant professor of radiology, developed a set of criteria to distinguish tumors from other bright spots, using features such as the location and shape of the bright spot, the sharpness of its border and whether the brain tissue surrounding the bright spot appears displaced or compressed.
Using these criteria, co-first authors Jennifer Griffith, MD, PhD, and Stephanie Morris, MD, assistant professors of neurology and of pediatrics, and colleagues studied brain scans from children with NF1 performed at the School of Medicine from 2006 through 2016. They analyzed scans from 68 NF1 patients as well as 46 children without NF1 for comparison. Most of the children had undergone multiple scans, so the researchers examined a total of 190 brain scans from NF1 patients and 104 scans from children without NF1.
All but four (94 percent) of the children with NF1 had bright spots, and none of the children without NF1 did. Further, in 57 percent of the children with bright spots, at least one of the spots was deemed likely to be a tumor.
It is difficult to prove that the researchers correctly distinguished tumors from less worrisome bright spots. Doing so would require extracting bits of the bright spots for examination, which would not be practical. However, 10 of the children whose bright spots were classified as probable tumors underwent brain biopsies as part of their medical care, and all 10 were proven to be brain tumors. Furthermore, 28 percent of these probable tumors eventually required treatment, providing further evidence that they had been correctly classified. The remainder did not cause symptoms and did not require treatment.
Applying the new criteria to MRI scans will help physicians identify probable tumors, but that does not mean that all children with NF1 should be scanned regularly, the researchers cautioned.
“I am not advocating the frequent use of MRI scans in kids with NF1,” Gutmann said. “What we have learned from this study is how to more accurately interpret MRI scans in children with NF1, and to better decide which abnormalities are most likely tumors in need of medical surveillance.”
Source: Read Full Article



