Using the right test for the right person to detect bowel cancer

Despite Australia and New Zealand having one of the highest rates of bowel cancer in the world, most Australians are either not having the right type of bowel cancer screening or not having any screening at all.
About 95% of people with bowel cancer survive if it is identified early, so increased screening is vital to reduce both the number of people with colorectal cancer and stress on the health system.
Yet more than 60% of those at increased risk are not being screened and almost 20% of people at average risk are having unnecessary colonoscopies.
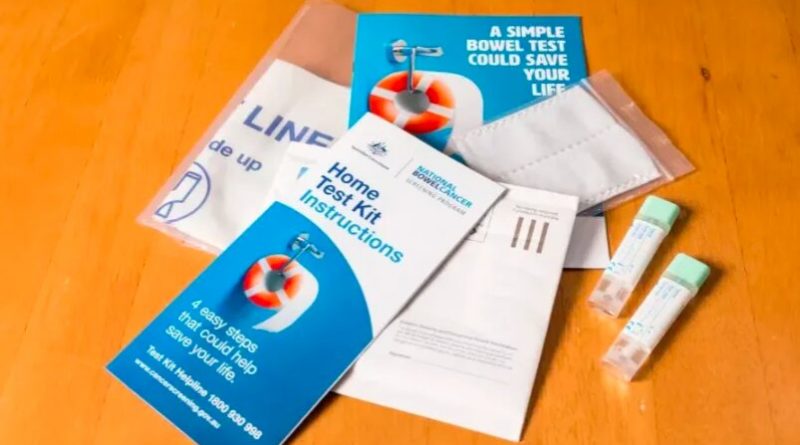
Every year, the National Bowel Cancer Screening Program (NBCSP) sends people aged 50 to 74 years the at-home National Bowel Cancer Screening Program immunochemical Fecal Occult Blood Test (iFOBT) or, as it’s affectionately known, the poo-test kit.
However, 59% of these tests are never returned and there is no screening program for those under 50.
With the incidence of early-onset bowel cancer increasing, we need to be able to capture those at increased risk and commence screening at an earlier age.
So how can screening be improved in the most impactful and cost-effective way?
To find out, our team tested a new method of risk-based colorectal cancer screening within a general practice setting—the first point of call for most of us when it comes to health. The results of the trial are published in the British Journal of General Practice.
The importance of risk-based screening
Risk-based screening is the way of the future, using more factors than age and family history to determine who needs further screening.
It was recently included as an objective in the draft 2023–33 Australian Cancer Plan to “support all Australians to access personalized, evidence-based cancer prevention and early detection strategies.”
In contrast, widespread population-level screening, where the fecal occult blood test kit is sent to everyone aged 50–74, is not designed to identify people at higher risk of developing bowel cancer.
This means that those who might need colorectal cancer screening with a colonoscopy, because they are at higher risk of developing bowel cancer in the future, are not being recommended it.
Conversely, there are many who are at average risk of bowel cancer having unnecessary colonoscopies when the safer and less expensive fecal occult blood test would be sufficient.
Risk-based screening can also identify people at higher risk to start screening at a younger age, catching cancers earlier with the ability to significantly improve outcomes.
The colorectal cancer risk predictor tool (CRISP)
This is where the Colorectal cancer RISk Predictor tool (CRISP) comes in—a web-based risk assessment and decision support tool that improves appropriate screening for bowel cancer in a general practice setting, developed by Professors Jon Emery, Mark Jenkins, Adrian Bickerstaffe and teams.
CRISP calculates an individual’s personal five-year and lifetime risk of developing bowel cancer and will recommend and encourage the right type of screening for a person’s risk.
And recent research by our team shows how risk-based screening can effectively work in a general practice setting.
This is because CRISP accounts for more than just age and family history to assess someone’s risk of bowel cancer. It also includes lifestyle factors like smoking history, weight, diet, and use of medications like aspirin and calcium.
It presents information about the potential benefits and harms of different screening tests and recommends the most appropriate screening (such as the poo-test kit or a colonoscopy) at an individual rather than population level.
Using the CRISP tool has been shown to help people to complete the most appropriate type of screening according to their risk of bowel cancer in those who were due to be screened.
A randomized controlled trial implementing CRISP in GP settings showed that for those people who were due screening, the use of CRISP, being shown how to use the poo-test kit, an SMS reminder and encouragement from their GP resulted in 20% more people doing the appropriate bowel cancer screening.
While researchers recommend the implementation of CRISP within a general practice setting, the CRISP tool is freely available online, so individuals could use it to create a report as a starting point for conversations with their doctor.
By using CRISP in general practice, we hope to contribute to a whole-of-system change needed to help individual Australians access the right bowel cancer screening at the right time.
More information:
Jon D Emery et al, The Colorectal cancer RISk Prediction (CRISP) trial: a randomised controlled trial of a decision support tool for risk-stratified colorectal cancer screening, British Journal of General Practice (2023). DOI: 10.3399/BJGP.2022.0480
Journal information:
British Journal of General Practice
Source: Read Full Article