Treating monkeypox like an STI may help control the outbreak, but stigma is a danger
The recent monkeypox global outbreak, now declared by the World Health Organization as a Public Health Emergency of International Concern (PHEIC), is sadly yet another reason for society to stigmatize and discriminate against the LGTBQ2SA+ community. This is in part because it has been suggested that monkeypox is a sexually transmitted infection (STI).
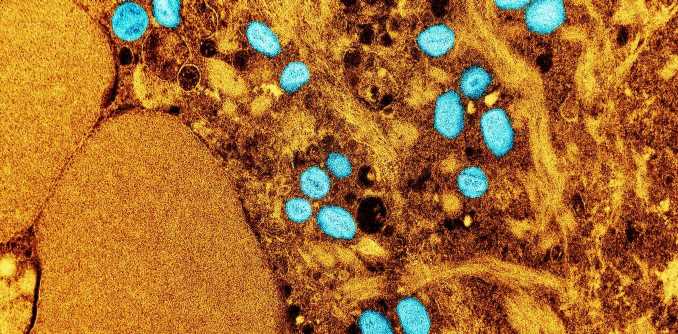
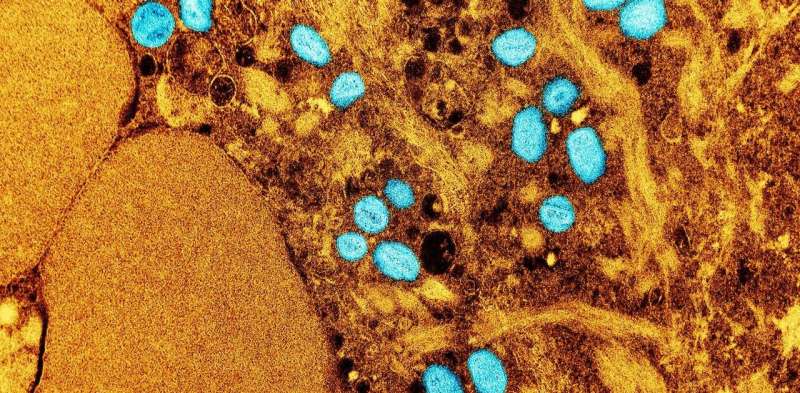
Monkeypox started as a zoonosis (an infection transmitted by contact with animals). However, this close relative of the variola virus (which causes smallpox) can also be transmitted from human to human, mainly through direct contact with the skin lesions.
Although transmission through semen and vaginal secretions has yet to be proven, it can be transmitted during sexual intercourse because of the obvious close contact it entails.
Cases have been identified for decades mainly in West African countries, but it was only recently when cases appeared in Europe and America that it caught the international attention it deserved. Cases continue to rise in many countries, to the point of prompting the WHO to declare it a PHEIC.
One excellent study put together a series of 500 patients distributed across 16 countries. The researchers analyzed patients’ demographics as well as their clinical characteristics. They found that 98% of the cases were men who prefer to have sex with men (MSM). Of note, 41% of the cases were people living with HIV (PLWH).
Characteristics of lesions
Another finding was the characteristics of the lesions. Monkeypox used to present with skin lesions mainly on the face, trunk, arms and legs, but most of the reported cases during this global outbreak have had a different presentation. Many cases have lesions in the perineal region (73%) or genitals or even around the mouth.
This could be consistent with sexual transmission as the lesions are presenting at the site of infection, a clinical course also described in this paper from Spain. Additionally, 30% of the patients also have another more common STI such as gonorrhea or syphilis, a pattern frequently found in many STIs. Managing a patient with an STI always implies ruling out other STIs.
Grouping diseases by their mode of transmission is helpful for doctors because it allows us to make mental lists of probable causes when confronted with a case. We call this differential diagnosis.
When a patient presents with a genital lesion, a health-care provider will establish a list of possible diagnoses based on the characteristics of the lesion, the accompanying symptoms and the local epidemiology. This makes it possible to treat empirically (before we can confirm the diagnosis) for the most probable cause.
What is an STI?
Any disease passed from one person to another through bodily fluids during a sexual encounter is considered an STI. However there are diseases that occur more frequently than others and as such are grouped in this category, such as chlamydia and gonorrhea.
Other diseases may be transmitted through genital secretions but are not considered an STI by the medical community. For example, Ebola has been shown to be transmitted through genital secretions, however it is not considered within the group of the more frequent STI because it is not its main mode of transmission.
The mode of presentation of monkeypox during this global outbreak has prompted the medical community to consider monkeypox diagnosis, along with other STIs, in any person who has had a recent unprotected sexual contact, and presents with a painful skin lesion in the genitals, perianal region or mouth.
Considering monkeypox as an STI seems logical in order to face the current outbreak, but the stigma and discrimination this could cause is a major problem. An infection acquired through sex is still something that causes guilt and fear of rejection by society. STIs are still viewed by many as a punishment for certain behaviors.
Additionally, classifying monkeypox as an STI may create a false sense of security for people who may think they’re not at risk. Both stigma and a low perception of risk can hinder efforts for early identification of cases, rapid isolation and limitation of the outbreak. Worst of all, stigma related to this outbreak would perpetrate harms to the LGTBQ2SA+ community.
Source: Read Full Article