Study examines role of socioeconomics in South African HIV infection rates
A team of McGill University researchers based at the Research Institute of the McGill University Health Centre (RI-MUHC) has reported survey results that show socioeconomics play a critical role in the detection, transmission and treatment of HIV in regions of South Africa.
In their study, Socioeconomic factors impact the risk of HIV acquisition in the township population of South Africa: a Bayesian Analysis, the researchers show those living in unstable housing conditions, such as hostels or informal dwellings, and those who had not completed post-secondary studies, were more likely to contract HIV.
Led by principal investigator Nitika Pant Pai, MD, Ph.D., an Associate Professor in the Department of Medicine and Cindy Leung Soo, a recent Master’s student now working at the Public Health Agency of Canada, the findings are published in PLOS Global Public Health.
The research adds to the existing analyses of HIV in South Africa in novel ways, Leung Soo says. “This study used data from a primary study which was conducted among participants in townships of Cape Town,” she explains.
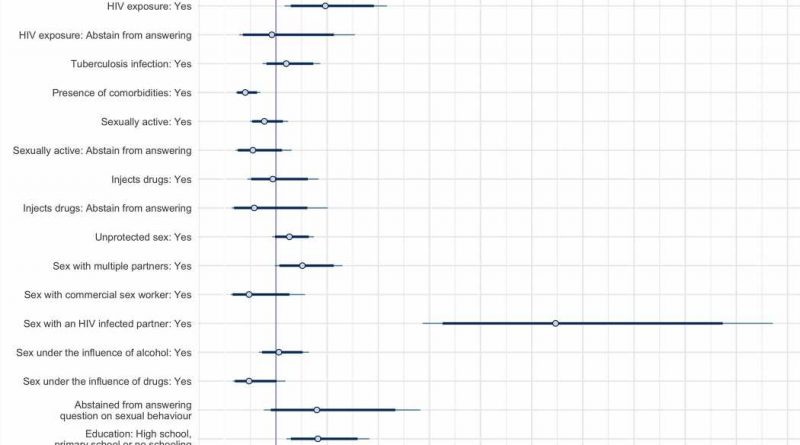
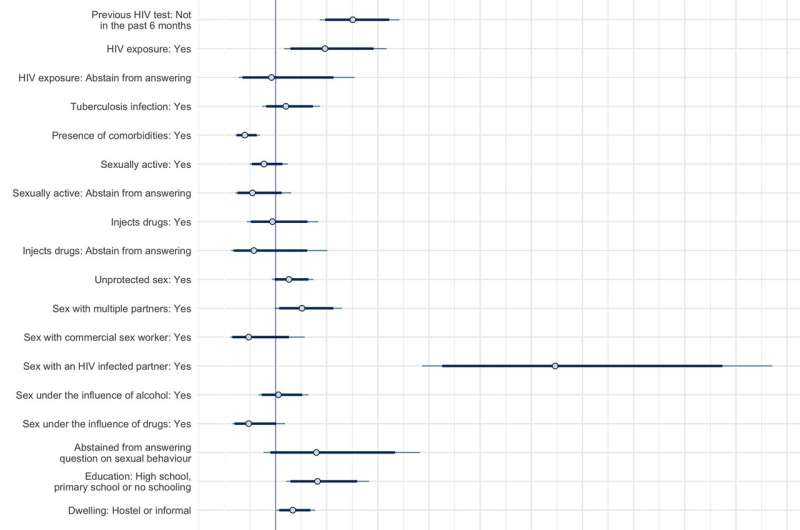
“We found that even within this relatively heterogeneous population, we can still find differences in HIV infection across different socioeconomic realities. Within our analysis, we controlled for behavioral and individual factors. We found that socioeconomic factors such as education and dwelling situations still impact HIV infection. We did a sex stratification within our analysis to elucidate how socioeconomic factors can impact HIV infections differently depending on whether they were male or female participants, and we found that they were impacted through different mechanisms in different ways.”
The team used Bayesian analysis, a method of statistical inference that allows researchers to combine prior information about a population parameter with evidence from information contained in a sample, to guide the statistical inference process.
“We dealt with missing data through multiple imputation. We used the observed data to impute the missing data, and then we conducted all our analysis within the Bayesian statistical framework, which offers us two key advantages,” explains Leung Soo.
“The first is it allows us to incorporate prior information. In our case, we used information from a study on the effects of age and sex on HIV infection to inform our prior understanding of how agents impact HIV infection. Secondly, the Bayesian statistical framework allows for more intuitive and meaningful interpretation of uncertainty intervals. That means the 89% credible intervals that are reported in the study are actual probability balance rather than confidence intervals, and they have a different interpretation, one that is more meaningful. It means the probability between X&Y is 89%.”
Reaching their conclusion
The findings show that socioeconomic factors impact HIV infections. “Even if we control for behavioral and individual factors, we saw that people who did not complete postsecondary education were 82% more likely to be infected with HIV compared to those who did have postsecondary education,” notes Leung Soo.
“But how these socioeconomic factors impact HIV is different between male and female participants. Among female participants, women who had lower education levels seem to be more likely to engage in certain sexual behaviors, such as having sex with multiple partners. Male participants who were living in less stable housing situations or who had lower education levels, appear to be less likely to have recently sought testing. It appeared that socioeconomic factors impacted their utilization of HIV services.”
According to Dr. Pant Pai, the data shows sexual behaviors and individual demographic factors alone cannot fully explain HIV infections. “Even when there is relative equity in health care, inequity remains a factor to be dealt with. Our findings invite us to reflect on how to address the HIV epidemic in South Africa and suggest that a greater focus on tackling social determinants of health, which fuel inequities in health, may be warranted.”
HIV testing is currently offered free of charge at local clinics in South Africa. Additionally, patients diagnosed with pulmonary tuberculosis are offered testing for HIV and all newly diagnosed pregnant or breastfeeding clients with an unknown or previously negative HIV status are also offered HIV testing services, notes Aliasgar Ismail, MD, Pulmonologist and study co-investigator from the University of Cape Town Lung Institute.
“There are limited community-based HIV testing services on offer, for example, there are stand-alone HIV testing sites located within the high burden communities. However, such services have the inadvertent drawback of perpetuating the stigmatization of people living with HIV. There are also some efforts by the local government to offer door-to-door HIV testing services, including, tracing of the sexual contacts of individuals who have tested positive for HIV. This strategy is effective but resource intensive.”
Pre-existing social conditions weigh heavily upon the management of HIV in the region says Dr. Pant Pai.
“In the South African context, they’re still dealing with the consequences of racism and apartheid. For example, in the case of the COVID-19 pandemic, there were separate rules in the provision of vaccines and food. The same thing applies to HIV. And as income inequality increases so does the rate of HIV infection. We found that the HIV risk in the townships varies and that men and women have different risks, and the risk of HIV really depends on their socioeconomic environment, which ties into their income, which ties into inequality, which ties into their education.”
“In the socioeconomic context, we certainly need to shift our focus. We must find out what is breeding and fueling HIV when women are poor and they are in abusive relationships they can’t get out of. Cindy’s work ties into what anthropologists have talked about for a very long time. Thankfully, all of this is now coming together to allow policymakers to say, ‘Hey, look, it’s extremely important to tackle the root cause of inequity,’ which is the relationship between uneven income distribution and health.”
More information:
Cindy Leung Soo et al, Socioeconomic factors impact the risk of HIV acquisition in the township population of South Africa: A Bayesian analysis, PLOS Global Public Health (2023). DOI: 10.1371/journal.pgph.0001502
Journal information:
PLOS Global Public Health
Source: Read Full Article