Stem cell-based implants successfully secrete insulin in patients with type 1 diabetes
Interim results from a multicenter clinical trial demonstrate insulin secretion from engrafted cells in patients with type 1 diabetes. The safety, tolerability, and efficacy of the implants, which consisted of pancreatic endoderm cells derived from human pluripotent stem cells (PSCs), were tested in 26 patients. While the insulin secreted by the implants did not have clinical effects in the patients, the data are the first reported evidence of meal-regulated insulin secretion by differentiated stem cells in human patients. The results appear December 2 in the journals Cell Stem Cell and Cell Reports Medicine.
“A landmark has been set. The possibility of an unlimited supply of insulin-producing cells gives hope to people living with type 1 diabetes,” says Eelco de Koning of Leiden University Medical Center, a co-author of an accompanying commentary published in Cell Stem Cell. “Despite the absence of relevant clinical effects, this study will remain an important milestone for the field of human PSC-derived cell replacement therapies as it is one of the first to report cell survival and functionality one year after transplantation.”
Approximately 100 years following the discovery of the hormone insulin, type 1 diabetes remains a life-altering and sometimes life-threatening diagnosis. The disease is characterized by the destruction of insulin-producing β-cells in the Islets of Langerhans of the pancreas, leading to high levels of the blood sugar glucose.
Insulin treatment lowers glucose concentrations but does not completely normalize them. Moreover, modern insulin delivery systems can be burdensome to wear for long periods, sometimes malfunction, and often lead to long-term complications. While islet replacement therapy could offer a cure because it restores insulin secretion in the body, this procedure has not been widely adopted because donor organs are scarce. These challenges underscore the need for an abundant alternate supply of insulin-producing cells.
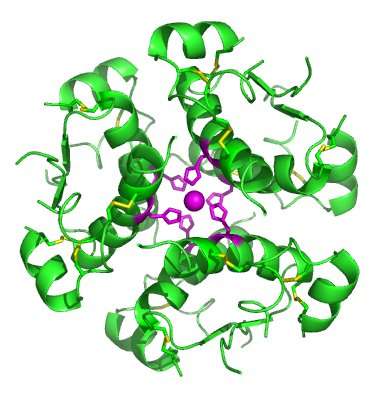
The use of human PSCs has made significant progress toward becoming a viable clinical option for the mass production of insulin-producing cells. In 2006, scientists at Novocell (now ViaCyte) reported a multi-stage protocol directing the differentiation of human embryonic stem cells into immature pancreatic endoderm cells. This stepwise protocol manipulating key signaling pathways was based on embryonic development of the pancreas. Follow-up studies showed that these pancreatic endoderm cells were able to mature further and become fully functional when implanted in animal models. Based on these results, clinical trials were started using these pancreatic endoderm cells.
Now two groups report on a phase I/II clinical trial in which pancreatic endoderm cells were placed in non-immunoprotective (“open”) macroencapsulation devices, which allowed for direct vascularization of the cells, and implanted under the skin in patients with type 1 diabetes. The use of third-party off-the-shelf cells in this stem cell-based islet replacement strategy required immunosuppressive agents, which protect against graft rejection but can cause major side effects, such as cancer and infections. The participants underwent an immunosuppressive treatment regimen that is commonly used in donor islet transplantation procedures.
In Cell Stem Cell, Timothy Kieffer of the University of British Columbia and his collaborators provided compelling evidence of functional insulin-secreting cells after implantation. PEC-01s—the drug candidate pancreatic endoderm cells produced by ViaCyte—survived and matured into glucose-responsive, insulin-secreting cells within 26 weeks after implantation. Over the up to one year of follow-up, patients had 20% reduced insulin requirements, and spent 13% more time in target blood glucose range. Overall, the implants were well tolerated with no severe graft-related adverse events.
“For the first time, we provide evidence that stem cell-derived PEC-01s can mature into glucose-responsive, insulin-producing mature β-cells in vivo in patients with type 1 diabetes,” Kieffer says. “These early findings support future investment and investigation into optimizing cell therapies for diabetes.”
However, two patients experienced serious adverse events associated with the immunosuppression protocol. Moreover, there was no control group and the interventions were not blinded, limiting causal conclusions, and outcomes were highly variable among the small number of participants. In addition, further studies need to determine the dose of pancreatic endoderm cells necessary to achieve clinically relevant benefits for patients.
In Cell Reports Medicine, Howard Foyt of ViaCyte and his collaborators reported engraftment and insulin expression in 63% of devices explanted from trial subjects at time periods ranging from 3 to 12 months after implantation. The progressive accumulation of functional, insulin-secreting cells occurred over a period of approximately 6-9 months from the time of implant.
The majority of reported adverse events were related to surgical implant or explant procedures or to immunosuppressive side effects. Despite potent systemic immune suppression, multiple surgical implantation sites, and the presence of foreign materials, the risk of local infection was exceedingly low, suggesting that this approach is well tolerated in subjects who are at risk for a poor healing response. The researchers are currently working on ways to promote graft vascularization and survival.
“The present study demonstrates definitively for the first time to our knowledge, in a small number of human subjects with type 1 diabetes, that PSC-derived pancreatic progenitor cells have the capacity to survive, engraft, differentiate, and mature into human islet-like cells when implanted subcutaneously,” Foyt says.
Both reports showed that the grafts were vascularized and that cells in the device can survive up to 59 weeks after implantation. Analyses of the grafts revealed that the main islet cell types, including β-cells, are present. Moreover, there was no formation of tumors called teratomas. However, the ratio of different endocrine cell types was atypical compared to mature pancreatic islets, and the total percentage of insulin-positive cells in the device was relatively low.
Regarding safety, most severe adverse events were associated with the use of immunosuppressive agents, emphasizing the life-long use of these drugs as a major hurdle for wider implementation of these types of cell replacement therapies. “An ideal and sunny possible future scenario would be the wide availability of a safe and efficacious stem cell-based islet replacement therapy without the need for these immunosuppressive agents or invasive, high-risk transplantation procedures,” says Françoise Carlotti of Leiden University Medical Center, a co-author of the related commentary.
According to de Koning and Carlotti, many questions remain to be answered. For example, researchers need to determine the differentiation stage at which the cells are most optimal for transplantation, and the best transplantation site. It is also not clear whether the effectiveness and safety of the cells can be maintained over time, and whether it is possible to eliminate the need for immunosuppressive therapy.
Source: Read Full Article



