Race, medicine and the future power of genetic ancestry
Writing in the New England Journal of Medicine that they “do not believe that ignoring race will reduce health disparities” but rather that “such an approach is a form of naive ‘color blindness’ that is more likely to perpetuate and potentially exacerbate disparities,” five Black geneticists set out to explain the pitfalls of leaving race out of medicine.
Importantly, the geneticists explain, while it is imperative to be considered now in many settings, race is an imperfect stepping stone toward the promise of using genetic ancestry for understanding health risks and tailoring treatments that will “improve Black health.” But there is a lot of work to be done for this future promise to be met.
UW news reached out to co-author Timothy Thornton, a UW statistical geneticist who is a professor, associate chair of education and director of graduate programs in the Department of Biostatistics, School of Public Health, to learn more:
UW News: Why write the article now? What is it that you were trying to capture about the moment we’re in?
Thornton: Recently there has been renewed interest in the medical community regarding the validity of considering race in clinical practice and healthcare. This debate has been sparked recently by the devastating effects of COVID, which is disproportionately affecting historically marginalized groups in the United States, such as Black Americans and Hispanics.
Some prominent voices have suggested that health disparities can be improved by providing uniform treatment regardless of race. In this article, however, we contend that ignoring race and using clinical algorithms and treatment guidelines based on studies of European ancestry populations can result in even greater health disparities in historically marginalized communities, such as Black Americans.
We also were compelled to write this article now because there is a dearth of Black scientists in the field of genetics and our voices really have not been heard on this topic. As five researchers in genetics who self-identify as Black men, we wanted to let the scientific community and the medical community know our perspective on the use of race in clinical practice and in biomedical research.
UW News: Why is your approach as put forth in the article important to bring into this conversation?
Thornton: I’m a statistical geneticist and my research is primarily focused on identifying and understanding the genetic components contributing to different health outcomes, and part of this recent discussion has been about the role of race: Is race only a social construct or is it something more than that?
We’re arguing in this article that race has a social component, but it also has a genetic component. Indeed, there are genetic differences between people belonging to different socially constructed racial categories. We think it’s important when we’re talking about race to acknowledge the genetic component as well as the social component.
We believe that there is a genetic component contributing to many health outcome differences we’re seeing by race and ethnicity. Differences in genetic architecture may increase the risk to COVID, for example, in addition to other factors, including co-morbidities and access to adequate healthcare. So, embracing genetic diversity in scientific research and in medicine is an important step to improving health outcomes and health disparities in marginalized communities.
UW News: What are some of the risks involved in including or leaving out race?
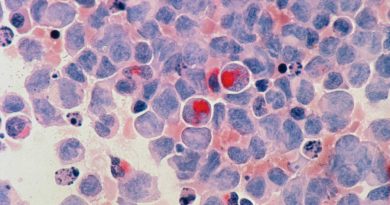
Thornton: Clinical algorithms—determining whether or not individuals should get a certain type of treatment—have largely been developed based upon people of European descent. Applying European-derived clinical algorithms to African Americans is not safe and can result in treatments that are actually harmful, as has been previously shown and that we highlight in our paper.
However, studies that include African Americans or other race/ethnicity groups can lead to medications or treatments that are specialized or tailored to a specific group, which can ultimately result in improved health outcomes. There are certain medications, for example, that have been found to work well in Black participants who were included in clinical trials and that never would have been identified if the results had not been stratified by race, because the drug didn’t do so well in European populations.
We’re trying to convey in this paper that ignoring race in medicine can be problematic and result in unintended consequences, particularly because there are huge health disparities by race in the U.S.; but if race is used appropriately, there is great potential for it to benefit everyone.
We also need to go beyond monolithic grouping of Black Americans. It is important to understand that the genetic ancestry of Black Americans is quite complex with substantial diversity in ancestry. Some Black Americans have more than 90% African ancestry, others actually have as little as 10% African ancestry. We also need to consider the non-negligible Native American ancestry contributions to many African Americans as well.
UW News: How should we view this complexity? How should it inform how we think about medical care?
Thornton: It’s a complex question as well because we’re still in the infancy of really understanding the genetic risk factors in diverse populations. What we’re largely trying to convey here is that there is a need for more studies that incorporate the diverse genomes of populations that are underrepresented in order to better understand risk.
A number of diseases have risk scores based upon a variety of behavioral factors, but we also need to consider contributions to risk scores based upon genetic factors.
Now there are risk algorithms that have been developed, called polygenic risk scores, for genetic factors, but once again they’ve largely been calculated using European studies and we need to build genetic risk scores based upon other populations.
We’re hoping the future of genomic medicine will appropriately incorporate diverse populations so we better understand why individuals from multiethnic populations with diverse genomes have different risk factors, beyond what can be explained by different behavioral risk factors.
UW News: How can health care professionals better communicate these risks and benefits to patients and their families?
Thornton: First, we need to be clear that there’s still a lot we do not know about the genetic components contributing to risk for a lot of diseases.
We know genetics plays a role in many health outcomes, with increased risk for certain people who have inherited certain genetic variants. In many cases, however, the genetic contributions can be small relative to the nongenetic factors including lifestyle characteristics, such as healthy eating, healthy living, exercise, socioeconomic status and access to affordable healthcare.
So, we need to be honest about what we know and what we don’t know, and I will say that there’s a lot more that we don’t know than we do know about genetic risk factors for many diseases.
And there’s even more that we don’t know about minority and marginalized populations, because they have not been studied very much. But as we get more studies, we will identify novel, new genetic risk factors in Black and other populations that have not been identified in European ancestry populations.
UW News: What about the concern of building even more stereotypes into the system? How would you talk to folks about using genetics without creating more labels about them?
Thornton: This question directly points to what we believe will be essential for personalized medicine of the future. Currently, clinical algorithms and treatment regimens that incorporate race often use self-reported monolithic race groups, saying, for example—a White individual with certain characteristics has a particular risk factor and/or recommended treatment. And there’s a different calculated risk and/or treatment for individuals who self-report to be Black.
Hopefully we will be able to get away from socially constructed racial groupings. Ideally, clinical algorithms and treatment guidelines should include genetic ancestry information in addition to, or in lieu of, race. However, we have not yet reached a point where genetic ancestry data are readily available in routine care or where clinicians know what to do with these data. Until then, we just cannot ignore race. We also can’t continue to extrapolate findings from studies in European populations and apply it to minority populations, because neither is going to be equitable or safe.
UW News: How can the health care system better serve Black patients, families and communities?
Thornton: There needs to be a concerted effort to include Black participants in clinical trials, so that we can identify more drugs that work well for this population. That’s the first thing. From the medical side, we need to be included in these clinical trials.
There also needs to be more Black participants included in research studies. I work in genetics and many of the genetic studies that I’ve been involved with have tens or even hundreds of thousands of individuals and only a small proportion of these individuals are non-European. We have to make an effort to do more studies in underrepresented minority populations and with a sufficient number of participants so that there is good chance of actually identifying something meaningful to improve health outcomes in these populations.
Third, we need to train more minority scientists and medical professionals, to guide and be involved in these studies and bring along the next generation.
Source: Read Full Article