Predicting suicide risk with the Oxford Mental Illness and Suicide (OxMIS) model
Researchers at the University of Oxford, Warneford Hospital, U.K., looking into a suicide prevention tool have published a paper titled “Predicting suicide risk in 137,112 people with severe mental illness in Finland: external validation of the Oxford Mental Illness and Suicide tool (OxMIS)” in the journal Translational Psychiatry. It details their efforts to retrospectively utilize a 17-question assessment tool as a predictor of suicide from a large cohort with severe mental illness (SMI).
Oxford Mental Illness and Suicide (OxMIS) tool is a free online standardized risk assessment tool that calculates suicide risk in patients with severe mental illness (schizophrenia-spectrum disorders or bipolar disorder) based on 17 sociodemographic, criminal history, familial and clinical risk factors.
To test the effectiveness of OxMIS, researchers compared the data of 137,112 people with severe mental illness (SMI) diagnosis in Finland between 1996 and 2017, of whom 101,655 (74%) were diagnosed with a schizophrenia-spectrum disorder and 35,457 (26%) with bipolar disorder.
One inpatient or outpatient episode per patient was randomly selected as the index episode out of the 5,261,732 episodes recorded. Each individual was assessed from the date of the random index episode for a 12-month follow-up period.
In the 12 months following their index episode, 1,475 individuals within this cohort died by suicide, representing a suicide prevalence rate of 1.1%. This probability was then used to interrogate the OxMIS tool.
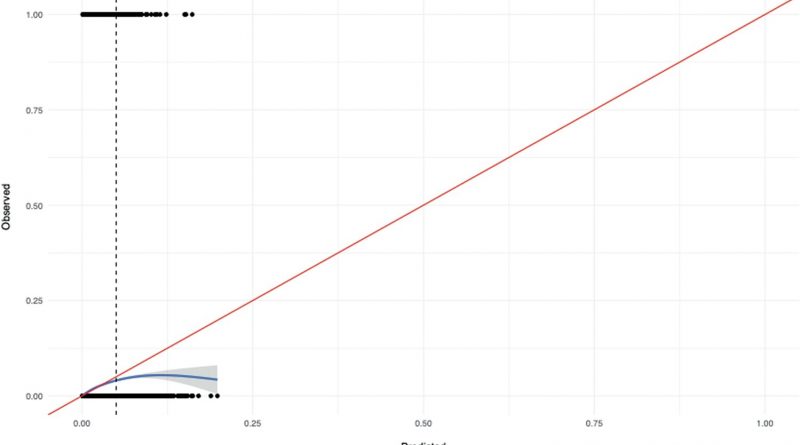
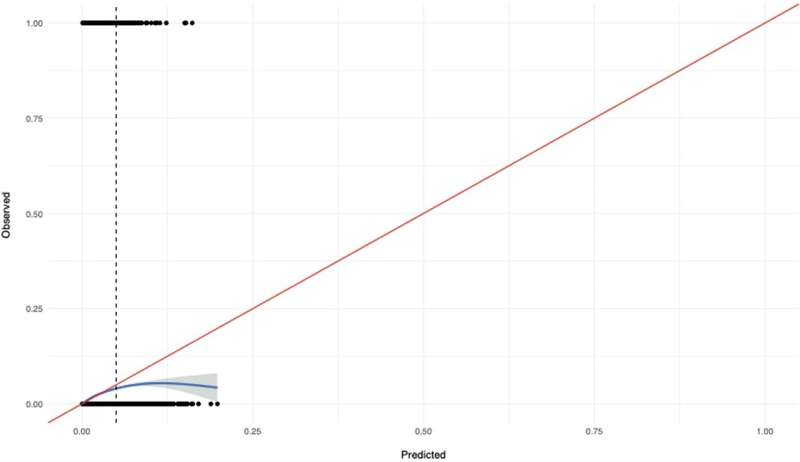
By randomly juxtaposing individuals who committed suicide with those who had not, OxMIS predicted a higher suicide risk score in 70% of suicides.
The model initially overestimated suicide risks in those with elevated predicted risks of greater than 5 % over 12 months, which applied to 1.3% (n = 1780) of the cohort. By tweaking the model predictions to a 5% maximum predicted suicide risk threshold (which is the clinically recommended protocol), the risk assessment accuracy improved, validating the clinical protocols and reinforcing that scores above 5% do not track well with increases in actual risk.
Validating clinical prediction tools requires rigorous methods and large data sets. The authors cite a recent study on the rapid proliferation of clinical prediction models in psychiatry, with only 16% having attempted independent validation and reported issues within those attempts. In the previous paper, “Clinical prediction models in psychiatry: a systematic review of two decades of progress and challenges,” published in Molecular Psychiatry, 94.5% of developed prediction models were identified as having a high risk of bias.
In the current study, researchers used a national register that allowed for the study of all individuals with SMI in the entire country of Finland over a 22-year period. The authors suggest that this method of validation, using routinely collected data, can address research gaps in prediction psychiatry and is a necessary step before translating such models into clinical practice.
More information:
Amir Sariaslan et al, Predicting suicide risk in 137,112 people with severe mental illness in Finland: external validation of the Oxford Mental Illness and Suicide tool (OxMIS), Translational Psychiatry (2023). DOI: 10.1038/s41398-023-02422-5
Journal information:
Translational Psychiatry
,
Molecular Psychiatry
Source: Read Full Article