Potential pancoronavirus fusion inhibitors that are effective against SARS-CoV-2 variants
Globally, the coronavirus disease 2019 (COVID-19) pandemic, which is caused by a novel coronavirus known as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has caused widespread suffering, death, and economic damage. This outbreak was declared a global pandemic by the World Health Organization (WHO) in March 2020.
SARS-CoV-2 is a single-stranded, positive-sense, enveloped ribonucleic acid (RNA) virus that belongs to the family Coronaviridae of the genus Betacoronavirus. Two other members of this family that have infected humans and caused significant outbreaks in the past decades include the severe acute respiratory syndrome coronavirus (SARS-CoV) in 2003 (China) and the Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012 (Saudi Arabia).
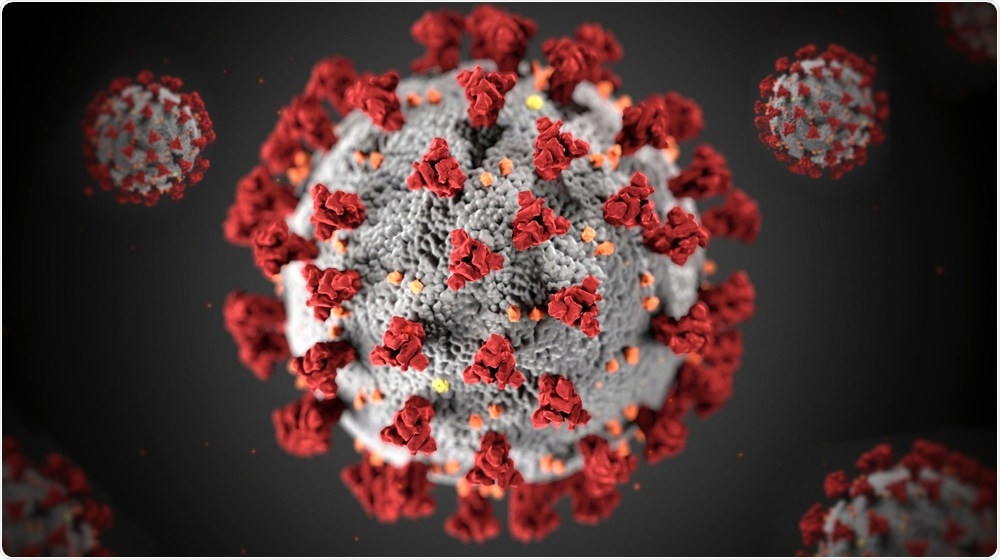 Study: Discovery of highly potent pancoronavirus fusion inhibitors that also effectively inhibit COVID-19 variants from the UK and South Africa. Image Credit: INSTANT Photography / Shutterstock.com
Study: Discovery of highly potent pancoronavirus fusion inhibitors that also effectively inhibit COVID-19 variants from the UK and South Africa. Image Credit: INSTANT Photography / Shutterstock.com
Why are vaccines and monoclonal antibody-based therapies are not enough to contain the COVID-19 pandemic?
Scientists worked at a tremendous speed and successfully developed several COVID-19 vaccines. Some vaccines, such as those developed by Pfizer-BioNTech, AstraZeneca, Moderna, Janssen Pharmaceutical Company of Johnson & Johnson, Sinovac, and Bharat Biotech, have already received emergency use authorization (EUA) from the global regulatory bodies. Despite this breakthrough, vaccines may not reach all people in the world.
Vaccine hesitancy is becoming and is expected to become a significant roadblock in getting the worldwide population vaccinated. In fact, Household Pulse Survey (HPS) results show that vaccine hesitancy in the United States is as high as 32%.
Vaccine hesitancy is defined as a delay in accepting or refusing vaccinations, despite the availability of vaccines. Vaccine hesitancy is complex and context-specific, varying across time, place, and vaccines.
The influences of vaccine hesitancy include complacency, convenience, fear of needles, or not understanding how vaccines work. This term covers delaying vaccinations, refusing vaccinations outright, and using certain vaccines while not others.
The emergence of SARS-CoV-2 variants has threatened the efficacy of existing vaccines. These vaccines have been developed against the spike (S) protein of the original strain of SARS-CoV-2 that was first reported in China in 2019, rather than that of the newly emerged variants.
Additionally, "breakthrough" cases of infection with COVID-19 have been reported among fully vaccinated individuals. Therefore, alternative treatments remain necessary and important.
In the United States, the Food and Drug Administration (FDA) has approved several monoclonal antibody-based treatments (e.g., Regeneron Pharmaceuticals and Eli Lilly) for emergency use; however, these treatments are prohibitively expensive and hard to access in most of the world.
Additionally, many of the monoclonal therapies were found to be ineffective against several SARS-CoV-2 variants that were recently identified in the United Kingdom, South Africa, and Brazil. Therefore, there remains an urgent need for alternative treatments that can aid in the fight against the ongoing pandemic.
Therapeutics and COVID-19
Although the U.S. FDA approved several repurposed drugs including remdesivir and lopinavir/ritonavir for the treatment of COVID-19, most clinical trials have shown that these drugs are not as effective as they were previously believed to be. Scientists claimed that although vaccines prevent severe COVID-19 disease and reduce the rate of mortality, therapeutics still play an important role for those individuals who experience vaccine breakthrough or when an unvaccinated individual gets infected.
In the current scenario, there remains a need for highly potent novel drugs with pancoronavirus activity and minimal toxicity. Importantly, scientists have identified many antiviral components against COVID-19 that are in their varied developmental phase that could play an important role in containing the pandemic.
Drugs that are targeted towards the receptor-binding domain (RBD) region of the S protein might lose their effectiveness over time, as this region is prone to undergo mutations. However, drug components that target the S2 domain of the S protein of SARS-CoV-2, which is a conserved region, may act as pancoronavirus inhibitors.
Pancoronavirus inhibitors
A new study published on the bioRxiv* preprint server has successfully identified and characterized a series of inhibitors that possesses pancoronavirus activity against SARS-CoV, SARS-CoV-2, and MERS-CoV. The authors of this study revealed that most active inhibitors could effectively restrict laboratory synthesized mutants. These synthesized mutants are similar to the variants that are dominantly circulating in the U.K. and South Africa.
In this study, the researchers reported a series of benzoic acid-based inhibitors with high pancoronavirus activity. Among the thirteen tested compounds, three compounds exhibited complete inhibition of virus-induced cytopathic effect (CPE) (IC100) at 1.25 micromolar (µM) against SARS-CoV-2 in vitro.
The researchers also found that the most active inhibitors could inhibit SARS-CoV-2 variants B.1.1.7 and B.1.351 that were originally identified in the U.K. and South Africa, respectively. The efficacy of these inhibitors was assessed in infected T cells that were transfected with the angiotensin-converting enzyme 2 (ACE2) receptors, which is the receptor used by SARS-CoV-2 to gain entry into cells. This inhibition was confirmed by low half-maximal inhibitor concentration (IC50) values upon exposure of the cells to these compounds.
Upon studying the mode of action of these pancoronavirus inhibitors through Surface Plasmon Resonance (SPR) imaging, the researchers reported that one of the most potent inhibitors binds to the prefusion S protein trimer of SARS-CoV-2. This technique also revealed that these drug components inhibit virus-mediated cell-cell fusion. Following the drug discovery protocol, researchers conducted in vitro Absorption, Distribution, Metabolism, and Excretion (ADME) studies, which revealed that all inhibitors possess potential drug-like characteristics.
Further investigation of the best inhibitor included in vivo pharmacokinetic studies using rats. These studies demonstrated an excellent half-life of 11.3 hours and a mean resident time (MRT) of 14.2 hours. These studies also revealed that some of the drugs are orally bioavailable.
Despite the presence of a rhodanine moiety, the researchers found that these inhibitors target the viral spike proteins and are not promiscuous or colloidal aggregators. Overall, the scientists are optimistic that these potent inhibitors would show high efficacy in preclinical and clinical trials.
“Overall, we discovered a set of novel small-molecule pancoronavirus fusion inhibitors, which are likely candidates with great potential to be developed as therapy of COVID-19 and related coronavirus diseases.”
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Curreli, F., Ahmed, S., Victor, S. M. B., et al. (2021) Discovery of highly potent pancoronavirus fusion inhibitors that also effectively inhibit COVID-19 variants from the UK and South Africa. bioRxiv. doi:10.1101/2021.09.03.458877. https://www.biorxiv.org/content/10.1101/2021.09.03.458877v1.
Posted in: Drug Trial News | Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibody, Cell, Coronavirus, Coronavirus Disease COVID-19, Drug Discovery, Drugs, Efficacy, Enzyme, Food, Imaging, in vitro, in vivo, Laboratory, Lopinavir, MERS-CoV, Metabolism, Molecule, Monoclonal Antibody, Mortality, Pandemic, Pharmaceuticals, Preclinical, Protein, Receptor, Remdesivir, Respiratory, Ribonucleic Acid, Ritonavir, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Therapeutics, Vaccine, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article



