Many big US cities now answer mental health crisis calls with civilian teams—not police

Christian Glass was a geology geek, a painter and a young man beset by a mental health crisis when he called 911 for help getting his car unstuck in a Colorado mountain town last year.
Convinced that supernatural beings were after him, he balked when sheriff’s deputies told him to get out of his car. The officers shouted, threatened and coaxed, body camera video shows. Glass prayed: “Dear Lord, please, don’t let them break the window.”
They did, and the 22-year-old grabbed a small knife. Then he was hit with bean bag rounds, stun gun charges and, ultimately, bullets that killed him and led to a murder charge against one deputy and a criminally negligent homicide charge against another.
As part of a $19 million settlement this spring with Glass’ parents, Colorado’s Clear Creek County this month joined a growing roster of U.S. communities that respond to nonviolent mental health crises with clinicians and EMTs or paramedics, instead of police.
The initiatives have spread rapidly in recent years, particularly among the nation’s biggest cities.
Data gathered by The Associated Press show at least 14 of the 20 most populous U.S. cities are hosting or starting such programs, sometimes called civilian, alternative or non-police response teams. They span from New York and Los Angeles to Columbus, Ohio, and Houston, and boast annual budgets that together topped $123 million as of June, The AP found. Funding sources vary.

“If someone is experiencing a mental health crisis, law enforcement is not what they need,” said Tamara Lynn of the National De-Escalation Training Center, a private group that trains police to handle such situations.
There’s no aggregate, comprehensive data yet on the programs’ effects. Their scope varies considerably.
In Denver, just an hour’s drive from where Glass was killed, a program called STAR answered 5,700 calls last year and is often cited as a national model. Its funding has totaled $7 million since 2021.
In New York, a more than $40 million-a-year program dubbed B-HEARD answered about 3,500 calls last year, and mental health advocates criticize it as anemic.
Representatives from some other cities were frank about challenges—staffing shortages, acclimating 911 dispatchers to sending out unarmed civilians, and more—at a conference in Washington, D.C., this spring.

Still, officials in places including New York see no-police teams as an important shift in how they address people in crisis.
“We really think that every single B-HEARD response is just a better way that we, the city, are providing care to people,” said Laquisha Grant of the New York Mayor’s Office of Community Mental Health.
Federal data is incomplete, but various studies and statistics show that mentally ill people make up a substantial proportion of those killed by police. Often, the dead are people of color, though Glass was not.
The alternative approach dates back decades but gained new impetus from calls for wide-ranging police reform after the 2020 killing of George Floyd in Minneapolis.
In Denver, STAR responders arrive in a van stuffed with everything from medical gear to blankets to Cheez-Its. In one recent instance, they spent three hours with a Denver newcomer who was living on the streets. The team helped him get a Colorado ID voucher, groceries, and medications and took him to a shelter.

“It’s really about meeting the needs of the community and making sure we are sending the right experts, so we can actually solve the problem,” says Carleigh Sailon, a former STAR manager who now works elsewhere.
STAR responded to 44% of calls deemed eligible last year, said Evan Thompkin, a STAR program specialist.
A Stanford University study found that petty crime reports fell by a third and violent crime stayed steady in areas that STAR served in its earliest phase. Throughout the program’s three years, police have never been called for backup due to safety concerns but have helped direct traffic, Thompkin said.
New York plans to expand its two-year-old B-HEARD program citywide. Officials note that its social workers and EMTs resolve about half of calls by talking to people or taking them to social service or community health centers, rather than hospitals.

Grant credits the program with “providing people with more options and letting people know that they can stay safely in their homes, in their communities, with the connection to the right resources.” Officials say B-HEARD answered 53% of “eligible” calls in the last six months of 2022, according to the most recent available data
But those calls are relatively few. Staffers answered about 2% of all mental health crisis calls citywide last year. Even within the program’s limited territory, it fielded 16% of such calls from July-December 2022.
Grant says the city is exploring whether more calls could qualify.
John Barrett, however, wanted to go to a hospital to get some physical and mental health problems checked out one June day. He asked 911 for an ambulance, but police came, he said. Then two other people showed up in bulletproof vests and face masks.
-

WellPower clinician Jane Lemaux loads supplies into a STAR van in Denver on Thursday, Oct. 20, 2022. The STAR program uses clinicians and EMTs or paramedics to respond to nonviolent mental health crises, instead of police. Data gathered by The Associated Press show at least 14 of the 20 most populous U.S. cities are hosting or starting such programs, sometimes called civilian, alternative or non-police response teams. They span from New York and Los Angeles to Columbus, Ohio, and Houston, and boast annual budgets that together topped $123 million as of June 2023, the AP found. Credit: AP Photo/Thomas Peipert
-

Activists participate in a rally to call for peer-led, non-police response to mental health crisis calls, Thursday, Sept. 29, 2022, in New York. The Associated Press has found that 14 of the 20 most populous U.S. cities are experimenting with removing police from some nonviolent 911 calls and sending behavioral health clinicians. Initiatives in major cities including New York, Los Angeles, Columbus, Ohio, and Houston had combined annual budgets topping $123 million as of June 2023. Credit: AP Photo/Mary Altaffer
-

Chris Richardson, associate director of criminal justice services at WellPower, is interviewed in Denver on Thursday, Oct. 20, 2022. WellPower’s STAR program uses clinicians and EMTs or paramedics to respond to nonviolent mental health crises, instead of police. Data gathered by The Associated Press show at least 14 of the 20 most populous U.S. cities are hosting or starting such programs, sometimes called civilian, alternative or non-police response teams. They span from New York and Los Angeles to Columbus, Ohio, and Houston, and boast annual budgets that together topped $123 million as of June 2023, the AP found. Credit: AP Photo/Thomas Peipert
-
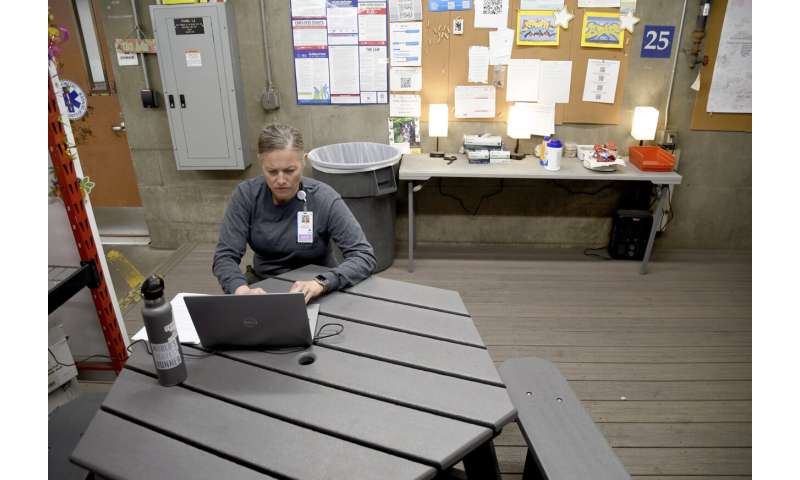
Leigh Foster, who supervises paramedics in Denver’s alternative policing program, works at an ambulance bay in the city on Thursday, Oct. 20, 2022. The STAR program uses clinicians and EMTs or paramedics to respond to nonviolent mental health crises, instead of police. Data gathered by The Associated Press show at least 14 of the 20 most populous U.S. cities are hosting or starting such programs, sometimes called civilian, alternative or non-police response teams. They span from New York and Los Angeles to Columbus, Ohio, and Houston, and boast annual budgets that together topped $123 million as of June 2023, the AP found. Credit: AP Photo/Thomas Peipert
-

Leah Faria, right, with the Woman’s Community Justice Association participates in a rally to call for peer-led, non-police response to mental health crisis calls, Thursday, Sept. 29, 2022, in New York. The Associated Press has found that 14 of the 20 most populous U.S. cities are experimenting with removing police from some nonviolent 911 calls and sending behavioral health clinicians. Initiatives in major cities including New York, Los Angeles, Columbus, Ohio, and Houston had combined annual budgets topping $123 million as of June 2023. Credit: AP Photo/Mary Altaffer
-

Keys hang on a wall at an ambulance bay in Denver on Thursday, Oct. 20, 2022. The city’s STAR program uses clinicians and EMTs or paramedics to respond to nonviolent mental health crises, instead of police. Data gathered by The Associated Press show at least 14 of the 20 most populous U.S. cities are hosting or starting such programs, sometimes called civilian, alternative or non-police response teams. They span from New York and Los Angeles to Columbus, Ohio, and Houston, and boast annual budgets that together topped $123 million as of June 2023, the AP found. Credit: AP Photo/Thomas Peipert
-

A woman walks past an ambulance bay as a STAR van exits in Denver on Thursday, Oct. 20, 2022. The STAR program uses clinicians and EMTs or paramedics to respond to nonviolent mental health crises, instead of police. Data gathered by The Associated Press show at least 14 of the 20 most populous U.S. cities are hosting or starting such programs, sometimes called civilian, alternative or non-police response teams. They span from New York and Los Angeles to Columbus, Ohio, and Houston, and boast annual budgets that together topped $123 million as of June 2023, the AP found. Credit: AP Photo/Thomas Peipert
-

Activist Ashley Conrad, foreground, participates in a rally to call for peer-led, non-police response to mental health crisis calls, Thursday, Sept. 29, 2022, in New York. The Associated Press has found that 14 of the 20 most populous U.S. cities are experimenting with removing police from some nonviolent 911 calls and sending behavioral health clinicians. Initiatives in major cities including New York, Los Angeles, Columbus, Ohio, and Houston had combined annual budgets topping $123 million as of June 2023. Credit: AP Photo/Mary Altaffer
“Between them and the police being there, I was just totally terrified,” recalled Barrett, 45, a former door technician.
He said he learned only by asking that they were with B-HEARD. (Teams can be summoned by on-scene police, and staffers are allowed to wear ballistic vests.)
The city mental health office said it couldn’t discuss any individual responses.
Barrett ultimately got an ambulance to a hospital.
“I’m saving money for an Uber next time,” he said.
© 2023 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed without permission.
Source: Read Full Article



