Good glycemic control in SARS-CoV-2 vaccinated type 2 diabetic patients reduces risk of breakthrough infection
A new study under consideration at a Nature Portfolio Journal and currently published on the Research Square* preprint server suggests that adequate glycemic control during the year after being vaccinated against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) improves the relative immunological response to the Pfizer-BioNTech messenger ribonucleic acid (mRNA) BNT162b2 vaccine and reduces the risk of coronavirus disease 2019 (COVID-19) breakthrough infections among type 2 diabetes (T2D) patients.

Study: Glycaemic control is associated with SARS-CoV-2 breakthrough infections in vaccinated patients with type 2 diabetes: an observational study. Image Credit: Andrey_Popov / Shutterstock.com
Factors associated with breakthrough SARS-CoV-2 infections
The global SARS-CoV-2 vaccination campaign has been very successful in reducing SARS-CoV-2 transmission and severity of COVID-19. However, a considerable number of breakthrough infections have emerged as a result of several factors, some of which include waning vaccine-induced antibody levels, the emergence of new viral variants with immune escape characteristics, and patient comorbidities. In particular, obesity, cardiovascular disease, and type 2 diabetes (T2D) are the most frequent comorbidities observed in fully vaccinated patients developing COVID-19.
T2D patients suffer from an undermined immune response with respect to both vaccination and natural infections. Glycemic control has been suggested to be the key determinant associated with the mounting of immune responses in T2D patients.
The association of glycemic control after SARS-CoV-2 vaccination with COVID-19 breakthrough infections is not yet clear. Thus, the researchers of the current study explored the possible association between glycemic control and immune responses after the BNT162b2 vaccination.
About the study
The current prospective observational study was conducted on healthcare and educator workers with T2D who had received the BNT162b2 vaccine. Subjects were followed up for an average of 346 days, during which they underwent five successive clinical, laboratory evaluations, and HbA1c assessments starting from the day of the second vaccine dose.
The one-year mean of HbA1c, which indicates the blood sugar levels in the past two to three months, from five successive visits was used as the metric of glycemic control to categorize the subjects into two groups. These two groups included those with poor glycemic control (PC) group, as defined as HbA1c less than 7%, and good glycemic control (GC) group, as defined as HbA1c exceeding 7%.
Neutralization antibody and T-cell responses were assessed in all participants after 14 days from the second dose and at each of the five visits. In addition, the team assessed who developed COVID-19 breakthrough infection more than 14 days after the second vaccine dose.
Cox regression analysis was used to examine the association between the one-year mean of HbA1c and survival from COVID-19 breakthrough infection and was adjusted for confounders including age, body mass index (BMI), diabetes duration, high-density lipoprotein (HDL)-cholesterol, cardiovascular risk factors, and active therapies.
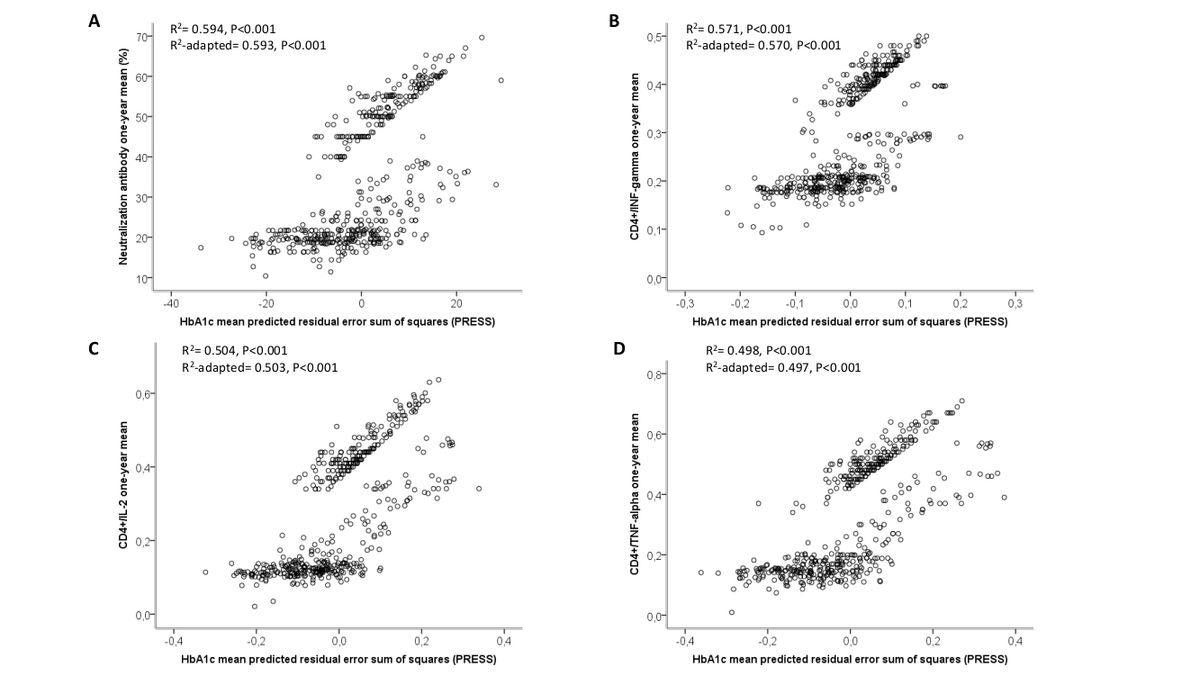
HbA1c has a significant relationship with vaccine-related immune parameters. Regression analysis between neutralization antibodies (A), CD4+/interferon-gamma (INF-gamma) (B), CD4+/interleukin-2 (IL-2) (C), CD4+/tumor necrosis factor-alpha (TNF-alpha) one-year mean (D) and HbA1c one-year mean (5 evaluations) predicted residual error sum of squares (PRESS).
GC T2D participants show better humoral and cell-mediated responses
Of the 494 participants, 196 were included in the GC group and 298 were categorized with PC. As assessed by the one-year mean of the percentage of neutralization, T2D patients with poor glycemic control showed a significantly reduced virus-neutralizing antibody capacity as compared to T2D patients with good glycemic control.
With regards to the cell-mediated immunity, the team observed a higher number of CD4+ T-helper cells expressing interferon (IFN)-γ, interleukin (IL)-2, and tumor necrosis factor-α (TNFα) in patients with good glycemic control as compared to patients with poorer control.
The one-year mean of HbA1c was found to be closely related with the one-year mean of antibody-mediated neutralization capacity and with the number of CD4+ T cells expressing IFN-γ, IL-2, and TNFα. Taken together, these findings support the hypothesis that glycemic control is closely related to the immune response elicited following SARS-CoV-2 vaccination.
Variables of ‘glycemia control’ and smoking impact breakthrough infections
The team recorded 10.5% and 3.6% breakthrough cases among T2D patients with PC and GC, respectively.
In addition, the one-year mean of HbA1c was significantly associated with the incidence of breakthrough infections with an adjusted hazard ratio (HR) of 0.285. Patients who reported a breakthrough infection exhibited significantly lower levels of both antibody-mediated neutralization capacity and CD4+ T cells expressing IFN-γ, IL-2, and TNFα during the peri-infection period.
In addition to glycemia, the only other factor associated significantly with the incidence of breakthrough infections was smoking with an HR of 0.360. As per previous studies, poorly controlled T2D and smoking are two of the major drivers of the debilitated immune system. Gradual deterioration of the immune system weakens the host's capacity to respond to infections as well as hinders the development of long-term immune memory.
In summary, our findings, coupled with the observation that achieving adequate glycemic control improves the relative immunological response, suggest that the implementation of diabetes care might enhance vaccine effectiveness, thus lowering the risk of SARS-CoV-2 breakthrough infection.”
*Important notice
Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Marfella R., Sardu, C., D’Onofrio, N., et al. (2022) Glycaemic control is associated with SARS-CoV-2 breakthrough infections in vaccinated patients with type 2 diabetes: an observational study. Research Square. doi:10.21203/rs.3.rs-1389539/v1, https://www.researchsquare.com/article/rs-1389539/v1
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Antibody, Blood, Blood Sugar, Body Mass Index, Cardiovascular Disease, CD4, Cell, Cholesterol, Coronavirus, Coronavirus Disease COVID-19, covid-19, Diabetes, Glycemia, HbA1c, Healthcare, Immune Response, Immune System, immunity, Interferon, Interleukin, Laboratory, Lipoprotein, Necrosis, Obesity, Research, Respiratory, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Smoking, Syndrome, T-Cell, TNFα, Tumor, Tumor Necrosis Factor, Type 2 Diabetes, Vaccine, Virus

Written by
Namita Mitra
After earning a bachelor’s degree in Veterinary Sciences and Animal Health (BVSc) in 2013, Namita went on to pursue a Master of Veterinary Microbiology from GADVASU, India. Her Master’s research on the molecular and histopathological diagnosis of avian oncogenic viruses in poultry brought her two national awards. In 2013, she was conferred a doctoral degree in Animal Biotechnology that concluded with her research findings on expression profiling of apoptosis-associated genes in canine mammary tumors. Right after her graduation, Namita worked as Assistant Professor of Animal Biotechnology and taught the courses of Animal Cell Culture, Animal Genetic Engineering, and Molecular Immunology.
Source: Read Full Article



