Genetic correlations between schizophrenia and eating disorders illuminated
Schizophrenia and eating disorders (EDs) are complex traits with considerable somatic and psychiatric morbidity, affecting 0.4–1% and 9% of the population, respectively. Risk for both is predominantly from genetic sources—64–81% for schizophrenia and 41–83% for EDs. Despite distinct diagnostic criteria and few common symptoms, significant genetic correlations between schizophrenia and anorexia nervosa (AN) have been identified in several recent genomic studies.
Still much is unknown about the genetic association between schizophrenia and other eating disorders than AN, and it is unclear if these disorders have common familial risks.
A new thesis by Ruyue Zhang, Ph.D. student at the Department of Medical Epidemiology and Biostatistics, aims to further our understanding of the underlying shared etiological pathway between schizophrenia and eating disorders. Ruyue has also studied the influences on clinical outcomes of EDs, and explores the impact of schizophrenia genetic risk on a wide range of medical conditions.
What are the main results in your thesis?
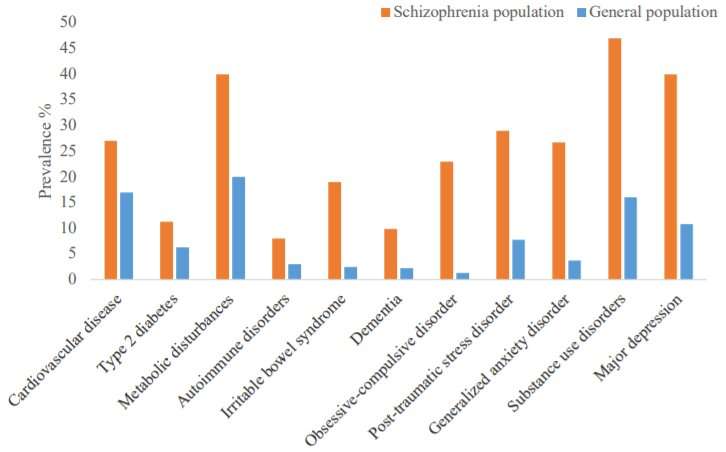
I found that individuals with AN or other types of eating disorders were at increased risk for having schizophrenia, and so were their relatives. But in general, the magnitude of risk decreased as genetic relatedness decreased. Thus, familial factors seem to contribute to the association between EDs and schizophrenia. We also found that family history of schizophrenia or schizophrenia genetic risk predispose individuals with AN to increased risk of psychiatric comorbidities but less severe ED-related symptoms. Moreover, our studies reveal that genetic risk for schizophrenia increases risk for a wide range of medical conditions including mental disorders, respiratory diseases, digestive diseases, etc. in individuals without schizophrenia.
Why did you choose to study this particular area?
I became interested in genetic epidemiology from the lectures given by Dr. Ralf Kuja-Halkola and Dr. Sarah Bergen during my master training. Luckily, I got the opportunity to work on a GWAS project related to bipolar disorders with Sarah. During the project work, I was intrigued by the challenges of diagnosing psychiatric disorders (compared to most of the somatic diseases) which are defined by reported or observed symptoms instead of pathologic evidence. This sparked my passion to learn more about psychiatric disorders. And at the same time, I was also impressed by a talk from Prof. Cynthia Bulik about the latest findings from the first AN GWAS which triggered my interest in deciphering the etiological overlap among psychiatric disorders. I would say it was perhaps a fortunate coincidence to become interested and step into this particular area.
What do you think should be done moving forward in this research area?
Source: Read Full Article



