Africa pins hopes on ‘breakthrough’ malaria vaccine

A ground-breaking vaccine against malaria has stoked hopes in Africa of rolling back a disease that claims hundreds of thousands of lives a year, many of them youngsters.
Since 2019, Ghana, Kenya and Malawi have immunised more than 800,000 children under a pilot programme using the RTS,S vaccine.
It is the first to show significant protection against the parasite-borne disease, cutting the risk of severe malaria by 30 percent, trials have shown.
On October 9, the World Health Organization (WHO), after sifting through the results of the pilot scheme, recommended the vaccine for children aged above five months in locations with malaria risk.
Some 260,000 children under five die from malaria each year in Africa, which accounts for about 90 percent of the global caseload.
“From a scientific perspective this is a massive breakthrough,” said Pedro Alonso, director of the WHO Global Malaria Programme.
Djermakoye Hadiza Jackou, coordinator of Niger’s National Malaria Control Programme (PNLP), said the WHO announcement was “welcomed with great joy.”
“This is something that was eagerly awaited.”
‘Super excited’
Pointing to a major issue in vaccine rollouts, the WHO said it found “strong” public demand for the jab. The vaccine is made by the British pharmaceutical giant GlaxoSmithKline (GSK), with the commercial name of Mosquirix.
Many parents who spoke to AFP also warmly supported the vaccine, although some were hesitant about possible side effects.
“I’m super excited about it,” said Hajia Aminu Bawa in southern Ghana’s Gomoa region, the mother of an 11-month-old girl.
“My child took the vaccine and nothing happened… I want to encourage every family with children below age two to go for the vaccine because it will go a long way to save lives.”
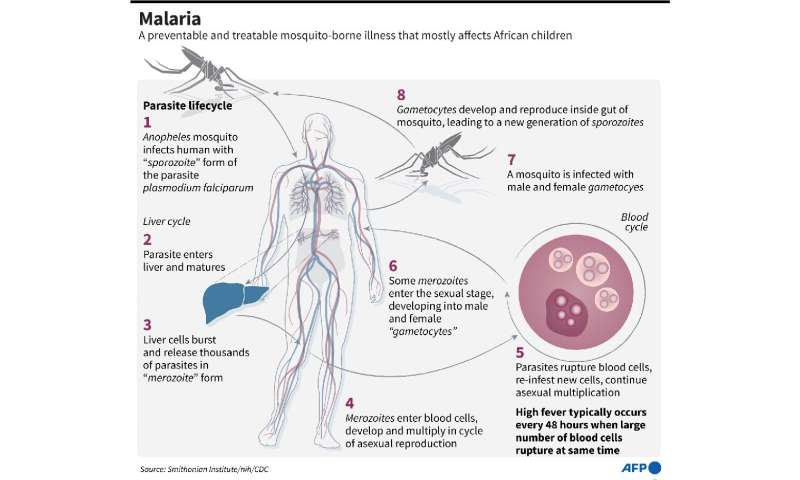
The vaccine aims to trigger the immune system to defend against the first stages of malaria.
The WHO says that the main side effects can include soreness at the injection site and fever, a similar reaction seen in other vaccines given to children.
Prince Gyamfi, the mother of a six-month-old boy in Gomoa, said she didn’t hesitate to get her child vaccinated.
“I have read about vaccines and how they work. I voluntarily came to vaccinate my child and so far nothing has happened,” she said.
“Some people discouraged me from giving him the vaccine because they said it’s new and can kill him but I think they said it out of ignorance.”
In Niger, which was not included in the pilot programme, AFP spoke to a mother named Fati, who was waiting outside a private clinic in Niamey, where her child was hospitalised with a new bout of malaria.
“When the vaccine arrives, it will be a great relief,” she said.
“Malaria kills our children and it doesn’t spare their parents, either.”

Unhealthy conditions
In neighbouring Burkina Faso, another vaccine developed by Britain’s University of Oxford in cooperation with the US firm Novavax has also shown promising effectiveness after a clinical trial in 2019.
But Niger’s Jackou and others cautioned against reliance on just a partial vaccine shield.
It is crucial to maintain time-honoured prevention techniques such as distributing insecticide-treated bed nets and early use of drugs to treat infection, they said.
In Burkina Faso’s capital Ouagadougou, these methods have been widely introduced since 2014, “reducing malaria-linked deaths by 25 to 30 percent,” said Wilfried Sawadogo, a local doctor.
Another enduring problem in malarial regions in sub-Saharan Africa is drainage—fighting the conditions that enable the Anopheles mosquito to breed and spread the parasite when it bites a human for a meal.
“If we die of malaria in Africa, it is because we live in totally unhealthy conditions, which means mosquitoes,” said Ousmane Danbadji, a sanitation specialist in Niger.
Who will pay?
The WHO announcement has raised the big issues of access to money and technology.
“Who is going to finance (a rollout)? Is the international community willing? That’s the first question. And will there be sufficient quantities?” asked Serge Assi, a researcher at the Pierre Richet Institute in Bouake in central Ivory Coast.
Christian Happi, director of the African Centre of Excellence for Genomics of Infectious Diseases in Ede, southwest Nigeria, said it was time for Africa to manufacture the vaccine and not just buy it.
“It is now up to Africa to grasp this technology, this knowledge, and produce vaccines rather than import them,” he said.
Source: Read Full Article



