What is Postural Orthostatic Tachycardia Syndrome (POTS)?
Causes and symptoms
Epidemiology
Diagnosis and treatment
References
Further reading
Postural orthostatic tachycardia syndrome (POTS) is a common heterogeneous form of cardiovascular autonomic dysregulation. The exact cause of POTS remains unclear. Patients typically complain of weakness, dizziness, rapid heartbeat, and palpitations when standing. Women in their adolescence or early adulthood, who are often in the middle of education or beginning their jobs, constitute the majority of those affected by POTS. The disorder can be highly disabling and financially ruinous.

Image Credit: Creative Cat Studio/Shutterstock.com
Causes and symptoms
The etiology of POTS is mainly unclear. Different theories surrounding the syndrome's genesis have been developed due to the heterogeneous symptomatology, early age at the beginning, and the presence of potential triggers in the patient's past. The three primary hypotheses are that POTS is either an autoimmune condition with unusually elevated sympathetic activity and excess catecholamines, a sympathetic denervation resulting in central hypovolemia, or a reflex tachycardia.
Early clinical observations indicated that the onset was comparable to Guillain-Barré syndrome and that the sickness frequently began with an acute infection, usually viral. This has drawn attention to the speculative but hardly ever substantiated notion of immunological involvement in POTS. This is backed by the fact that autoimmune diseases typically have female preponderance and temporal associations with prior virus infections, vaccinations, or trauma.
Additionally, POTS patients commonly display signs of immune system dysfunction and positive autoimmune test results. An autoimmune basis has been proposed as a possible cause of POTS. Several autoreactive IgGs have been discovered, including the ganglionic acetylcholine receptor (gAChR), voltage-gated potassium channel complex, and cardiac lipid raft-associated proteins.
Other suggested pathomechanisms include issues with autonomic cardiovascular control, abnormally elevated sympathetic activity, excess catecholamines in the blood, peripheral sympathetic denervation that causes central hypovolemia, and abnormally elevated sympathetic activity. This hypothesis proposes that peripheral sympathetic denervation would cause venous pooling and lower preload, which would result in compensatory heart rate elevation, while increased central sympathetic outflow would explain insufficient sinus tachycardia.
Chronic orthostatic intolerance is the hallmark and pathognomonic symptom of POTS, which is frequently made worse by additional factors like high ambient temperature, inadequate fluid intake, dehydration, physical strain, early morning hours, or fever.
However, POTS patients frequently experience a wide range of additional symptoms. Upon POTS first manifests, dizziness, weakness, a quick heartbeat, and palpitations when standing are the most often reported symptoms. Additionally, syncope, weariness, stomach pain, and headaches are noted.
It is unknown if extravascular volume depletion and deconditioning in patients with additional autonomic symptoms contribute to POTS, however, GI problems are persistent in POTS patients. The pathogenesis of POTS is complex and includes volume dysregulation, deconditioning, excessive sympathetic drive, and defective sympathetically mediated vasoconstriction.
Epidemiology
Postural orthostatic tachycardia syndrome, one of the most widespread types of orthostatic intolerance in the world, the prevalence ranges between 0.2% and 1.00% in developed countries. It is estimated to impact about 500000 patients in the United States. POTS primarily affects younger people, with an 80 percent female gender predominance. Young, premenopausal Caucasian girls between the ages of 15 and 45 make up the vast majority of POTS patients, with the bulk of cases being diagnosed between the ages of 15 and 25.
Diagnosis and treatment
When evaluating a patient with suspected POTS, it's important to confirm the diagnosis, look for comorbid disorders, and rule out anything that could be the origin of or closely resemble the autonomic syndrome. Orthostatic intolerance symptoms, the severity and scope of other autonomic conditions, further potential arrhythmia, potential contributing effects of medications or dietary supplements, and other comorbid diseases must be established by a thorough clinical history.
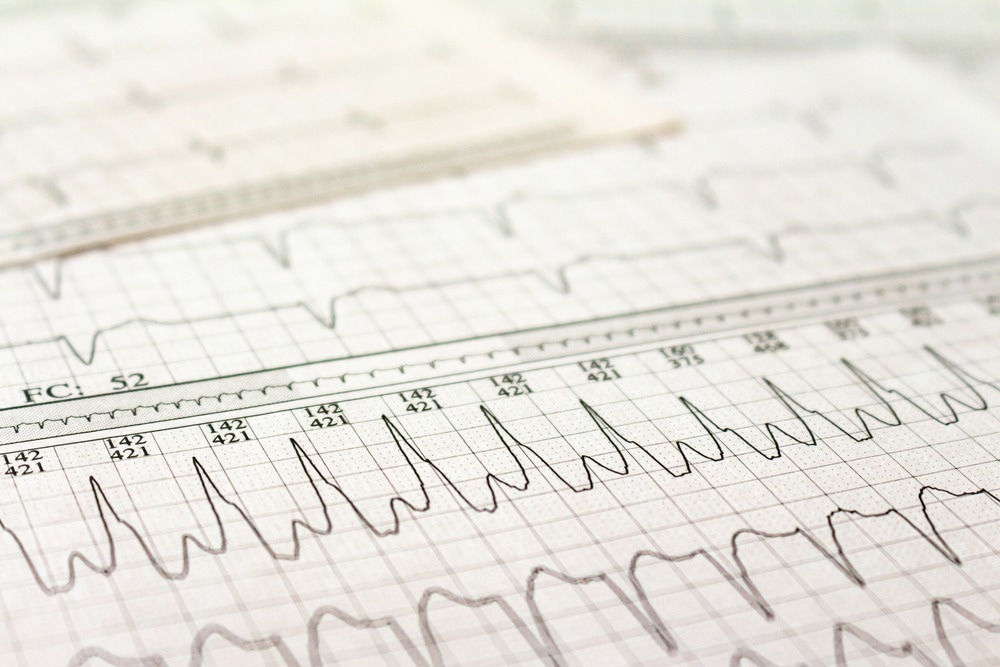
Image Credit: Horacio Selva/Shutterstock.com
For clinicians and affected patients, the heterogeneity and broad spectrum of POTS-related symptoms present a significant problem. Additionally, due to POTS' poorly understood pathophysiology, treating the disease's underlying causes is practically impossible, and care of the condition is typically centered on symptom relief. POTS' long-term prognosis has not been thoroughly studied.
About half of all POTS patients are thought to spontaneously recover between one and three years. An accurate diagnosis is the first step in the proper management of POTS. The syndrome should be fully explained to patients. After the diagnosis, the patient should get full education regarding non-pharmacological treatments that relieve symptoms, long-term prognosis, and therapy options suitable for the patient's condition.
Paying proper attention to the environment's temperature, engaging in strenuous exercise, or right after eating can prevent acute exacerbation of symptoms. Medications that aggravate orthostatic tachycardia and sinus tachycardia should be stopped when possible. Among them are norepinephrine reuptake inhibitors and stimulant medicines.
Typically, medical professionals evaluate various medications to reduce heart rate, enhance peripheral vasoconstriction, and boost intravascular volume. However, pharmacological therapy only has limited overall results, and even when multiple medicines are used, the disease still profoundly impacts the most symptomatic patients.
Exercise that improves cardiovascular fitness and steps to raise effective blood volume is also crucial. Non-pharmacological therapies can be sufficient in some situations. Additionally, medical facilities and professional bodies need to ascertain whether the diagnostic criteria for POTS, which are overly comprehensive, have caused a problem since they have an extremely "high" diagnostic sensitivity but relatively low diagnostic specificity.
References
- Zhao S, Tran VH. Postural Orthostatic Tachycardia Syndrome. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541074/
- Vernino, S., Bourne, K. M., Stiles, L. E., Grubb, B. P., Fedorowski, A., Stewart, J. M., Arnold, A. C., Pace, L. A., Axelsson, J., Boris, J. R., Moak, J. P., Goodman, B. P., Chémali, K. R., Chung, T. H., Goldstein, D. S., Diedrich, A., Miglis, M. G., Cortez, M. M., Miller, A. J., Freeman, R., … Raj, S. R. (2021). Postural orthostatic tachycardia syndrome (POTS): State of the science and clinical care from a 2019 National Institutes of Health Expert Consensus Meeting – Part 1. Autonomic neuroscience : basic & clinical, 235, 102828. https://doi.org/10.1016/j.autneu.2021.102828
- Olshansky, B., Cannom, D., Fedorowski, A., Stewart, J., Gibbons, C., Sutton, R., Shen, W. K., Muldowney, J., Chung, T. H., Feigofsky, S., Nayak, H., Calkins, H., & Benditt, D. G. (2020). Postural Orthostatic Tachycardia Syndrome (POTS): A critical assessment. Progress in cardiovascular diseases, 63(3), 263–270. https://doi.org/10.1016/j.pcad.2020.03.010
- Watari, M., Nakane, S., Mukaino, A., Nakajima, M., Mori, Y., Maeda, Y., Masuda, T., Takamatsu, K., Kouzaki, Y., Higuchi, O., Matsuo, H., & Ando, Y. (2018). Autoimmune postural orthostatic tachycardia syndrome. Annals of clinical and translational neurology, 5(4), 486–492. https://doi.org/10.1002/acn3.524
- Fedorowski A. (2019). Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management. Journal of internal medicine, 285(4), 352–366. https://doi.org/10.1111/joim.12852
- Dahan, S., Tomljenovic, L., & Shoenfeld, Y. (2016). Postural Orthostatic Tachycardia Syndrome (POTS)–A novel member of the autoimmune family. Lupus, 25(4), 339–342. https://doi.org/10.1177/0961203316629558
Further Reading
- All Heart Content
- Structure and Function of the Heart
- An Overview of Aortic Dissection
- What is Cardioprotection?
Last Updated: May 3, 2023
Source: Read Full Article



