Program that trains community health workers to deliver hearing care shows success among low-income older adults
A first-in-kind program that trains trusted older adult community health workers to fit and deliver low-cost hearing technology to peers with hearing loss significantly improved communication function among participants, according to the results of a randomized clinical trial led by Johns Hopkins Medicine researchers.
According to the National Institutes of Health, two-thirds of adults 70 and older have clinically significant hearing loss, but less than 20% of adults with hearing loss use a hearing aid. Rates of hearing aid use are even lower among low-income adults, often due to the high cost of devices, limited insurance coverage and inadequate access to hearing care professionals. Racial and ethnic health inequities also contribute to low levels of hearing aid use among older African Americans with hearing loss.
Hearing loss isn’t just an inconvenience that comes with getting older—it’s a critical public health issue that is now the focus of national and international initiatives coming from the national academies, the White House and the World Health Organization. This global attention to hearing loss is the result of the growing understanding of the impact that hearing loss can have on the risk of dementia, cognitive decline, greater health care costs and other adverse outcomes.
To bridge this gap in access to hearing care, Johns Hopkins Medicine researchers developed HEARS (Hearing health Equity through Accessible Research and Solutions) to train community health workers (CHWs) to work one on one with their peers living in affordable independent housing.
The CHWs, trained and supervised by local audiologists, conducted two-hour sessions with clients, counseling them about the basics of age-related hearing loss and communication strategies, then delivering and fitting them with low-cost, over-the-counter amplification devices provided by the HEARS program.
Otologist Carrie Nieman, M.D., M.P.H., core faculty at the Johns Hopkins Cochlear Center for Hearing and Public Health, first author of the clinical trial and co-creator of the HEARS model, said the program is not intended to replace audiologists and otolaryngologists who have specialized training in hearing loss.
The goal instead, she said, is to “recruit and train community health workers who share some of the same lived experiences as those who go without hearing care, which represents the vast majority of older adults with hearing loss. From this position, CHWs can gain trust and connect with their clients in ways that hearing care professionals, like myself, often cannot.”
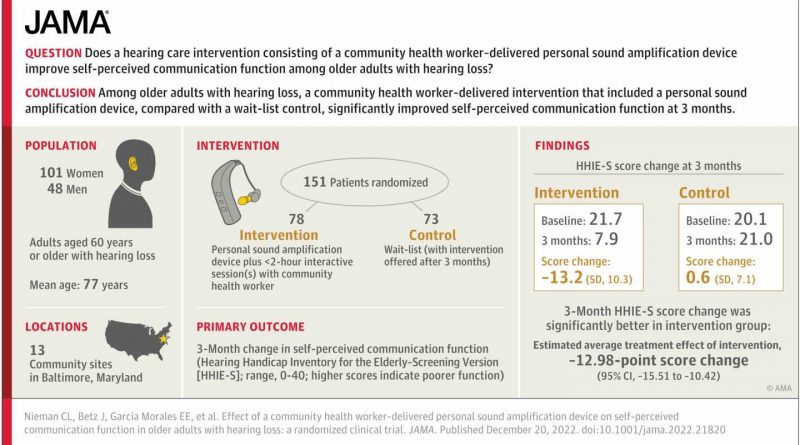
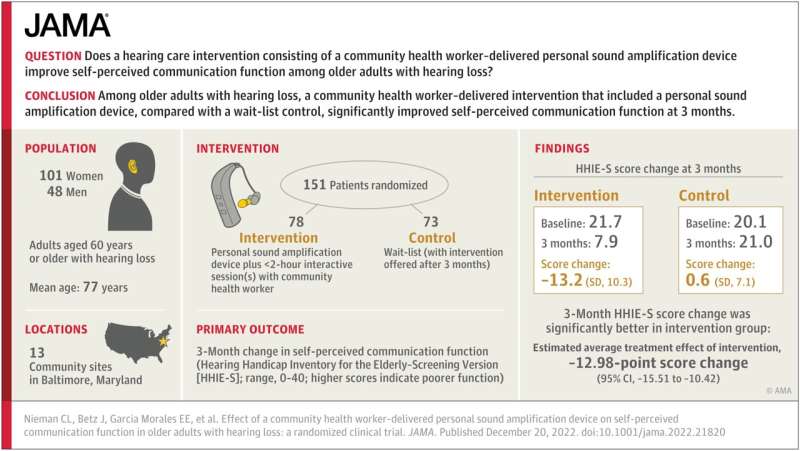
In this trial, researchers recruited 151 participants from 13 community sites in Baltimore, Maryland, which included affordable independent housing complexes and senior centers. A randomized group of 78 people received a CHW-led hearing care intervention, while a waitlist control group of 73 people did not. The average age of participants was 76.7 years old, 101 participants were women and 65 identified as African American. Two-thirds of participants were in the low-income bracket, and nearly half did not have or use a smartphone.
Communication function, a measure of the impact of hearing loss on an individual’s daily communication, was assessed for all participants through a commonly used tool known as the Hearing Handicap Inventory. Scoring on the measure ranges from zero to 40, with higher scores indicating more communication difficulty.
Those who received help from a CHW had a baseline median score of 21.7 and a median score of 7.9 at a three-month follow-up visit with the CHW. By contrast, the waitlist control group saw little to no change, with a baseline median score of 20.1 and a median score of 21 at the three-month follow-up.
Overall, the researchers say, the results of the trial, published in the Journal of American Medical Association (JAMA), revealed that participants reported significant improvement after a three-month follow-up compared with the control group. Results suggest that those who worked with a CHW experienced benefits from the two-hour hearing intervention session that were similar in magnitude to what is reported in the literature for hearing aids fit by an audiologist.
“They came to us and received help from us because we are just like them—we are seniors,” said Renee Hicks, a CHW who provided hearing devices and education to her peers. “They would learn from us because we were living in the same community. It helped health-wise, too; people were coming out of their apartments and participating in activities.”
“This trial validates a model of hearing care that empowers community health workers to reach older adults with untreated hearing loss. The HEARS program connects individuals with a hearing device and needed education,” said Nieman. “The reach of the HEARS program is amplified by newly available over-the-counter hearing aids, providing older adults the tools they need to age well.”
Nieman says further trials of the HEARS program are planned at three sites across Maryland, and is seeking collaborators to grow the program globally.
More information:
Carrie L. Nieman et al, Effect of a Community Health Worker–Delivered Personal Sound Amplification Device on Self-Perceived Communication Function in Older Adults With Hearing Loss, JAMA (2022). DOI: 10.1001/jama.2022.21820
Journal information:
Journal of the American Medical Association
Source: Read Full Article