mAb treatment can rapidly select for SARS-CoV-2 resistance, suggests study
Monoclonal antibody (mAb) therapy is currently given to non-hospitalized persons with early severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and mild to moderate coronavirus disease 2019 (COVID-19). Several SARS-CoV-2 mutations have emerged after the introduction of mAbs for treatment. However, there is a lack of evidence suggesting that the SARS-CoV-2 resistance mutations can lead to altered viral replication dynamics or loss of therapeutic efficacy.
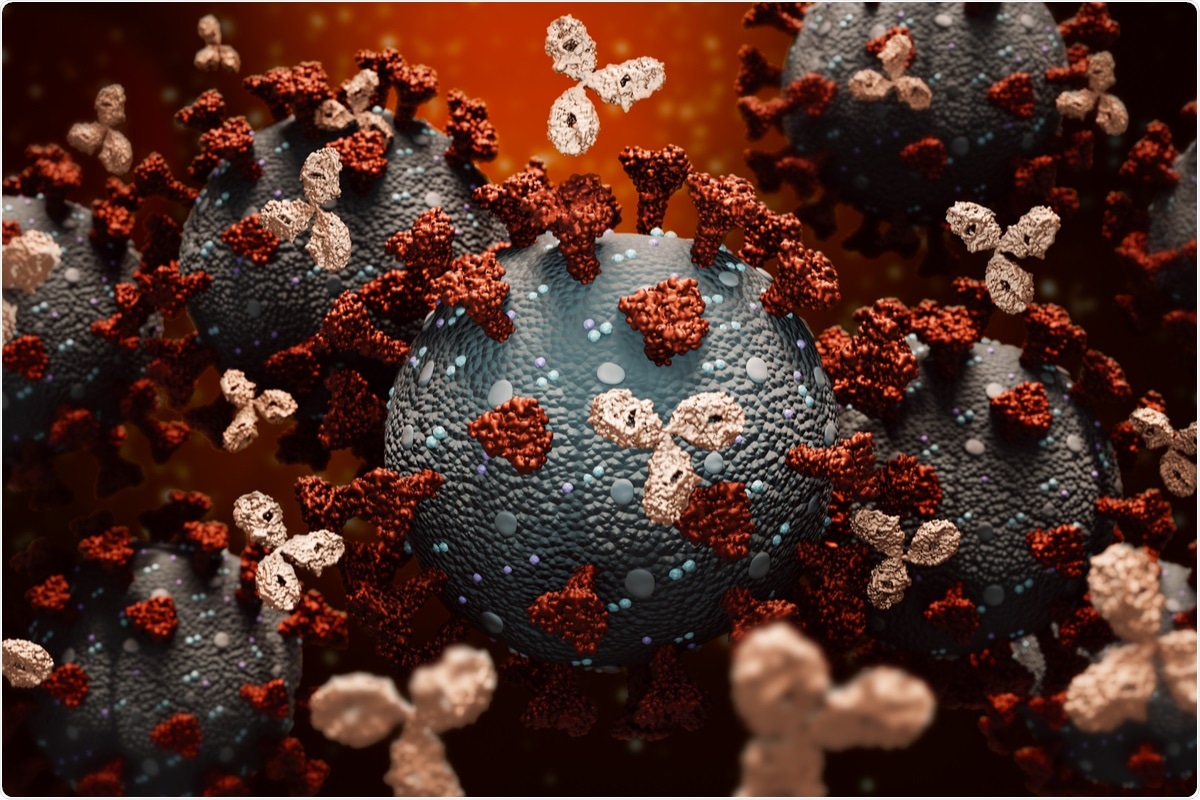 Study: Emergence of SARS-CoV-2 Resistance with Monoclonal Antibody Therapy. Image Credit: MattLphotography/ Shutterstock
Study: Emergence of SARS-CoV-2 Resistance with Monoclonal Antibody Therapy. Image Credit: MattLphotography/ Shutterstock
A study available on the preprint server medRxiv* evaluates the efficacy of a mAb to prevent disease progression in non-hospitalized persons with symptomatic SARS-CoV-2 infection. This study reports the emergence of SARS-CoV-2 resistance mutations in the host upon mAb treatment and their effect on viral load dynamics, symptom severity, and treatment efficacy.
A preprint version of the study is available on the medRxiv* server, while the article undergoes peer review.
Bamlanivimab
Bamlanivimab was the first monoclonal antibody approved by the US Food and Drug Administration (FDA) for emergency use authorization (EUA). A clinical study showed that treatment with bamlanivimab decreased detection of SARS-CoV-2 in nasal swabs. It also reduced the risk of hospitalization and death.
ACTIV-2/A5401 trial
ACTIV-2/A5401 is a clinical trial listed on ClinicalTrials.gov. It is a study to evaluate the safety and efficacy of different antiviral agents to prevent disease progression in non-hospitalized persons with symptomatic SARS-CoV-2 infection. Bamlanivimab is one of the antiviral agents tested in this study.
In this phase 2 randomized trial, participants were randomized to receive an intravenous infusion of bamlanivimab or a placebo. Adults 18 years old or above with a positive SARS-CoV-2 antigen test and nucleic acid or PCR test were enrolled in the study if the sample was collected within ten days of symptom onset
Bamlanivimab recipients either received 7000 mg mAb or 700 mg mAb. Of the 95 participants randomized to receive 7000 mg, 48 received treatment, and 46 received placebo. This dosing group was halted because another study showed that bamlanivimab 700 mg and 7000 mg have similar efficacy. The 700 mg study group had 223 participants; 111 received treatment and 112 received placebo. The research staff collected nasopharyngeal (NP) swab samples on days 0, 3, 7, 14, and 28 of the study. The participants self-collected daily anterior nasal (AN) swabs until day 14 and at days 21 and 28 of the study.
Simultaneously, the participants were monitored for 13 symptoms: fever, cough, shortness of breath or difficulty breathing, sore throat, body pain or muscle pain or aches, fatigue, headache, chills, nasal obstruction or congestion, nasal discharge, nausea, vomiting, and diarrhea.
The NP and AN swab samples were tested for viral load, and the viral spike protein was sequenced for identifying mutations.
The emergence of resistant mutations
In the bamlanivimab 700 mg treatment group, treatment-emergent resistance mutations were detected in 7% of participants. There were no treatment-emergent mutations among the 48 participants that received bamlanivimab 7000 mg. The emergence of SARS-CoV-2 resistance mutations was associated with a relatively consistent change in viral load kinetics. The participants detected with emerging mAb resistant virus had significantly higher pre-treatment NP and AN viral load.
The respiratory tract of the participants was intensively sampled, and it revealed the dynamic nature of SARS-CoV-2 evolution. There was a rapid and sustained viral rebound after the emergence of resistance mutations. This also correlated with symptom severity. It is important to note that there was no difference observed in the severity of symptoms between the treatment and placebo groups before the emergence of resistant mutations.
When the resistance mutations started emerging in the participants of the bamlanivimab 700mg treatment group, the AN viral load increased significantly, and the symptoms gained severity simultaneously.
The emerging mAb resistant virus also accumulated additional mutations found in current variants of concern and variants of interest. These mutations were apart from the bamlanivimab site of activity and may reflect an attempt to escape from host immunity.
Limitations and implications
Clinically, bamlanivimab is now used in combination with other agents. Even then, these results provide proof of principle for the role of drug resistance in the clinical efficacy of anti-SARS-CoV-2 therapies. A lack of treatment-emergent mutations was found in the 7000 mg group. This may be because of the limited sample size of this phase 2 study, especially in the bamlanivimab 7000 mg group.
For optimal therapeutic benefit, it is recommended that mAb treatment be initiated during the early stages of infection. The findings of this study suggest that there is a potential risk with mAb treatment due to the emergence of resistance mutations. The insights gained from this study could design anti-SARS-CoV-2 therapeutics while preventing the emergence of viral resistance.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Choudhary, M. et al. (2021) "Emergence of SARS-CoV-2 Resistance with Monoclonal Antibody Therapy". medRxiv. doi: 10.1101/2021.09.03.21263105.
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibody, Antigen, Breathing, Clinical Trial, Coronavirus, Coronavirus Disease COVID-19, Cough, Diarrhea, Efficacy, Evolution, Fatigue, Fever, Food, Headache, immunity, Monoclonal Antibody, Muscle, Nausea, Nucleic Acid, Pain, Placebo, Protein, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sore Throat, Spike Protein, Syndrome, Therapeutics, Throat, Virus, Vomiting
Written by
Dr. Shital Sarah Ahaley
Dr. Shital Sarah Ahaley is a medical writer. She completed her Bachelor's and Master's degree in Microbiology at the University of Pune. She then completed her Ph.D. at the Indian Institute of Science, Bengaluru where she studied muscle development and muscle diseases. After her Ph.D., she worked at the Indian Institute of Science, Education, and Research, Pune as a post-doctoral fellow. She then acquired and executed an independent grant from the DBT-Wellcome Trust India Alliance as an Early Career Fellow. Her work focused on RNA binding proteins and Hedgehog signaling.
Source: Read Full Article



